BJU International:吸烟会增加患者接受前列腺癌治疗的风险
2015-02-03 MedSci MedSci原创
图 1 前列腺特异性抗原无复发存活率(P=0.003) 图2 吸烟情况的无癌转移存活结果 图3 吸烟与胃溃疡毒性(P=0.02) 在前列腺癌患者中,接受治疗的吸烟患者有增加副作用的风险,并且未来有癌症复发的可能性,甚至会死于前列腺癌。研究结果发表在《英国泌尿科期刊》上,研究表明吸烟可能对前列腺癌患者的健康状况产生负面影响,并导致相关的并发症。 几项研究已经证实吸烟和
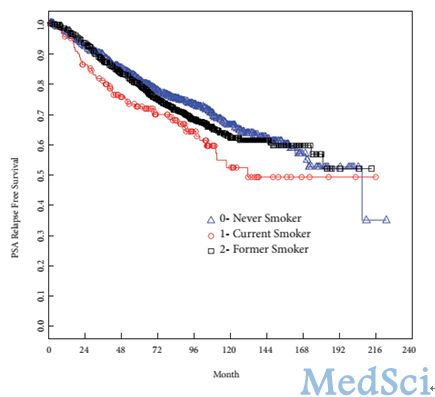
图 1 前列腺特异性抗原无复发存活率(P=0.003)
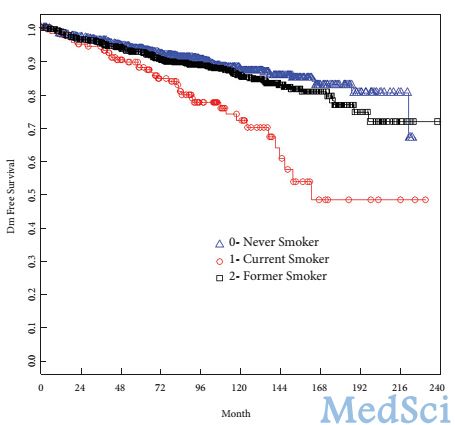
图2 吸烟情况的无癌转移存活结果
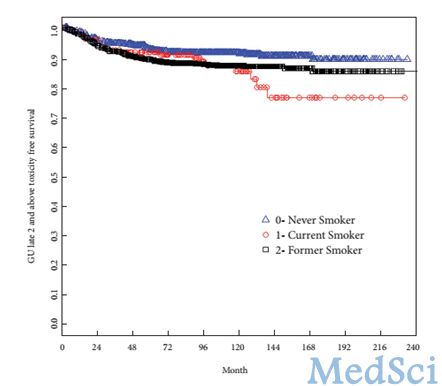
图3 吸烟与胃溃疡毒性(P=0.02)
在前列腺癌患者中,接受治疗的吸烟患者有增加副作用的风险,并且未来有癌症复发的可能性,甚至会死于前列腺癌。研究结果发表在《英国泌尿科期刊》上,研究表明吸烟可能对前列腺癌患者的健康状况产生负面影响,并导致相关的并发症。
几项研究已经证实吸烟和前列腺癌之间的联系。为了更好地理解吸烟对前列腺癌发展进程和治疗的影响,纽约纪念斯隆凯特林癌症中心放射肿瘤学教授医学博士Michael Zelefsky和他的同事研究了1988年到2005年之间2358例接受外部光束放射治疗前列腺癌的患者。其中,2156名有吸烟史。患者将不吸烟者,当前吸烟者,先前吸烟者,当前吸烟未知者进行分类。
随访近八年来,当前吸烟的患者相比于从未吸烟的患者,癌症复发风险增加了40%,癌症扩散和死亡的风险也增加了近2倍。此外,当前吸烟的患者和先前吸烟的患者出现副作用的可能性较高,如尿毒性等。
当前吸烟的患者会显著增加前列腺特异抗原复发的风险(危害比 HR 1.4, P = 0.02),转移的风险(HR 2.37, P < 0.001),前列腺癌死亡的风险(HR 2.25, P < 0.001)。多变量分析表明,吸烟与放射治疗相关的生殖泌尿毒性的风险增加也有关联(当前吸烟的患者,HR 1.8,P = 0.02;先前吸烟的患者 HR 1.45,P = 0.01)。吸烟不会增加胃肠道毒性。
原始出处
Emily Steinberger, Marisa Kollmeier, Sean McBride, Caroline Novak, Xin Pei, Michael J. Zelefsky. Cigarette smoking during external beam radiation therapy for prostate cancer is associated with an increased risk of prostate cancer-specific mortality and treatment-related toxicity. BJU International, 2015; DOI: 10.1111/bju.12969\
本文是MedSci编译,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











这篇文章有一定深度
94
是一篇不错的文章
88
戒烟难
72
#Nat#
31
#eRNA#
37
这个研究有特色
111