盘点:多发性骨髓瘤近期重要研究进展一览
2017-10-29 MedSci MedSci原创
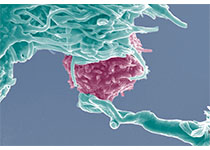
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里梅斯小编整理了近期关于多发性骨髓瘤的指南及重要研究新进展与各位一
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里梅斯小编整理了近期关于多发性骨髓瘤的指南及重要研究新进展与各位一同分享。
【1】pomalidomide、bortezomib和dexamethasone联合治疗复发性多发性骨髓瘤的最大耐受剂量、疗效和安全性
研究人员设计一I/II期试验对pomalidomide(泊马度胺), bortezomib(硼替佐米)和dexamethasone(地塞米松)(PVD)联合治疗复发性来那度胺耐受性的多发性骨髓瘤(MM)的最大耐受剂量(MTD)、安全性和疗效。结果表明,PVD是治疗复发性来那度胺耐受性的多发性骨髓瘤(MM)的有效方案。逐周加大硼替佐米的剂量不仅可以耐受而且方便。毒性副作用是可控的,大多都是轻度血细胞减少,没有明显神经病变。
【2】Ricolinostat联合硼替佐米以及地塞米松治疗复发或难治性多发性骨髓瘤
抑制组蛋白脱乙酰基酶(HDAC)可以增强蛋白酶体抑制作用治疗多发性骨髓瘤的疗效,但是也会增加毒性。临床前研究发现HDAC6通过蛋白质降解过程中的聚集体/自噬途径调节蛋白体酶抑制抵抗。CLIN CANCER RES近期发表了一篇文章,报道HDAC6选择性抑制剂Ricolinostat的临床试验结果。研究主要观察Ricolinostat的安全性、初步疗效以及联合标准蛋白酶体抑制治疗的Ⅱ期试验推荐剂量。结果表明,Ricolinostat的Ⅱ期临床试验推荐剂量为160mg每天,与硼替佐米及地塞米松联合治疗安全、耐受性良好,并且具有活性,表明HDAC6选择性抑制是治疗多发性骨髓瘤的可行途径。
【3】VSIG4是多发性骨髓瘤独立预后指标
近期,发表于oncotarget的一篇文章中,研究人员评估了VSIG4在MM患者的表达及其对预后影响。研究人员对81例骨髓和66例MM患者的髓外活检样本进行了免疫组化检测,并与MMGP的VSIG4 mRNA表达数据进行结合分析。结果显示,VSIG4高表达组的总生存期(OS)显著低于VSIG4低表达组,分别对rISS和mSMART风险分类进行调整后,VSIG4表达水平仍具有统计学意义。在髓外MM患者和MMGP的外部数据中分析VSIG4的表达情况也得到该结果。表明VSIG4是MM预后不良的独立指标,这意味着VSIG4或是MM的免疫治疗靶点。
【4】嵌合抗原受体(CARs)为多发性骨髓瘤带来新的治疗前景
现在为止,多发性骨髓瘤(MM)几乎是一种不可治愈的浆细胞(B细胞)恶性肿瘤,因此探索新的治疗方式迫在眉睫。T细胞疗法是一种新的有望治愈MM的方法,其作用机制与现有的MM的标准疗法不同。MM抗体,包括CD138、CD38、SLAMF7和κ轻链,均作为CAR靶点进行研究。MM是基因和表现均为杂合,因此靶向多个抗原或许可以提高CAR T细胞治疗MM的效果。CAR T细胞联合其他骨髓瘤疗法将成为未来研究的主要领域。虽然治疗MM的CAR T细胞疗法仍处于初始研究阶段,但已经展现出其可提高MM治疗效果的巨大前景。
【5】卡非佐米和硼替佐米用于复发性或难治性多发性骨髓瘤的疗效对比
3期ENDEAVOR试验对两种蛋白酶体抑制剂用于复发性或难治性多发性骨髓瘤的疗效进行对比。已报道的中期分析表明卡非佐米联合地塞米松的无进展生存期明显优于硼替佐米联合地塞米松。现进行二次中期分析来比较两个治疗组之间的总体生存期的情况。研究从多个地区多家医院和诊所招募年满18岁的已接受过1-3次治疗的复发性或难治性多发性骨髓瘤患者。结果表明,与硼替佐米相比,卡非佐米具有重要的临床意义性的降低死亡风险的特点。
【6】抗癌新药开辟多发性骨髓瘤治疗新策略
肿瘤形成多发性骨髓瘤是非常具有挑战性的治疗,仍被认为是不可治愈的。在最近发表的科学杂志“Oncotarget”的研究中,乌普萨拉大学的研究人员显示蛋白质BMI-1的抑制作用如何可以用作治疗疾病的新策略。在本研究中,研究人员已经研究了蛋白质BMI-1作为新的多发性骨髓瘤疗法的潜在靶标。当它们在培养的骨髓瘤细胞中抑制BMI-1时,发现细胞的活力降低,并且更大百分比的细胞停止分裂并死亡。此外,抑制BMI-1与多发性骨髓瘤中先前确定的药物靶标的组合增强了单一目标抑制介导的抗骨髓瘤作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#多发性#
24
好文章学习了
35
#研究进展#
15
谢谢分享
38
学习了受益匪浅
30
学习
46