以精神异常起病的双侧丘脑梗死2例报告
2019-11-12 李乐 余丹芳 张帆 中国实用神经疾病杂志
双侧丘脑梗死是一种少见的脑卒中类型,患者多存在血管变异。小部分人丘脑穿通动脉(丘脑旁正中动脉)起源于单侧大脑后动脉,这种变异血管被称为Percheron动脉,该动脉闭塞所致的双侧丘脑梗死在缺血性脑卒中患者中占0.1%~2%。Percheron动脉脑梗死不仅发病率低,临床症状也较特殊,主要表现为意识障碍、精神智能障碍、垂直性凝视麻痹。现将湖北省中西医结合医院近期收治的2例以精神异常起病的Perche
双侧丘脑梗死是一种少见的脑卒中类型,患者多存在血管变异。小部分人丘脑穿通动脉(丘脑旁正中动脉)起源于单侧大脑后动脉,这种变异血管被称为Percheron动脉,该动脉闭塞所致的双侧丘脑梗死在缺血性脑卒中患者中占0.1%~2%。Percheron动脉脑梗死不仅发病率低,临床症状也较特殊,主要表现为意识障碍、精神智能障碍、垂直性凝视麻痹。现将湖北省中西医结合医院近期收治的2例以精神异常起病的Percheron动脉脑梗死病例报道如下。
1.临床资料
病例1:男,63岁,因“突发行为异常1d”于2016-04-19入院,表现为突起胡乱吃药、一反常态夜晚欲外出跑步,重复吐痰、冲水,不听家人劝说等。既往有高血压、房颤、脑梗死史,发病前无感染、精神受刺激等诱因。入院体检:体温36.5 ℃,心率78次/min,呼吸20次/min,血压125/68 mmHg(1 mmHg=0.133kPa),房颤律,轻度嗜睡,记忆力、计算力下降,言语混乱,无自知力,双侧瞳孔等圆等大,直径约4mm,对光反射灵敏,双侧眼球位置正常,向各方向活动正常,双侧面纹对称,伸舌居中,四肢肌力5级,肌张力正常,腱反射对称,病理征未引出,无感觉障碍,无共济失调。
入院血糖、血脂、肝肾功能检查正常。心电图显示心房纤颤。颅脑DWI示双侧丘脑、右顶叶急性脑梗死(图1)。脑常规MRA示双侧大脑中后动脉管腔粗细欠均,右侧大脑中动脉M2段管腔变窄。颈部血管彩超示左侧颈动脉粥样硬化斑块形成,左侧椎动脉管腔均匀性细窄,血流速度变慢。心脏彩超示左房扩大,室间隔增厚,室间隔活动幅度明显减低,左室后壁活动幅度代偿性增强,二尖瓣、三尖瓣反流,心律失常。入院后给予华法林抗凝、改善脑循环等治疗,治疗1个月精神症状减轻出院。
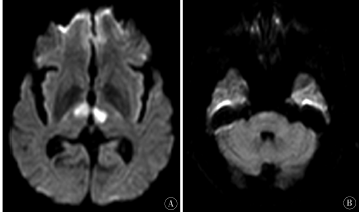
图1 病例1DWI显示双侧丘脑旁正中区受累,中脑未受累
入院体检:体温36.5℃,心率78 次/min,呼吸20 次/min,血压125/68mmHg,心律规整,轻度嗜睡,定向力、记忆力、计算力下降,无自知力,双侧瞳孔等圆等大,直径约4mm,光反射灵敏,双侧眼球位置正常,向各方向活动正常,双侧面纹对称,伸舌居中,四肢肌力5级,肌张力正常,腱反射对称,病理征未引出,无感觉障碍,无共济失调。
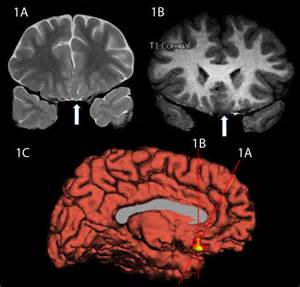
入院后血脂检查:TC 5.91mmol/L,TG0.82mmol/L,HDL 1.42mmol/L,LDL 3.1mmol/L。甲状腺功能:FT3 3.82 pmol/L,FT4 18.61pmol/L,TSH 0.092μIU/mL。心电图正常。颈部血管彩超示双侧颈动脉多发粥样硬化斑块形成,左侧椎动脉流速减低,阻力指数增高。心脏彩超示左室舒张功能减低。颅脑DWI示双侧丘脑急性脑梗死(图2)。脑常规MRA 示脑血管硬化改变。给予拜阿司匹林抗血小板、改善脑循环等治疗,治疗10d精神症状减轻出院。

图2 病例2DWI显示双侧丘脑旁正中区受累,中脑未受累
2.讨论
丘脑的血液由颈内动脉系统及椎基底动脉系统同时供应,主要为下侧动脉、旁正中动脉、丘脑结节动脉、脉络膜后动脉。Percheron 于1976年提出存在Percheron动脉的解剖变异,该动脉源于一侧大脑后动脉P1段,供应双侧丘脑旁正中区域及中脑嘴部。报道称约1/10的人存在此变异。Percheron梗死典型临床症状为意识障碍、精神智能障碍、垂直性凝视麻痹。旁正中区域主要包括背正中核和髓板内核,其经过丘脑脚与前、眶额和内侧前额叶皮质存在相互激活性连接(上行网状激活系统),因此,旁正中丘脑梗死常导致精神意识改变,如淡漠、嗜睡等。与丘脑相关的边缘叶纤维受损可引起记忆力改变。国外也有类似的以急性精神错乱起病的Percheron脑梗死报告。向上注视麻痹定位于中脑顶盖前区,向下注视麻痹定位于双侧丘脑中脑结合处,两部位受损可出现垂直性注视麻痹。中脑受累还可以出现运动障碍、共济失调等。
本文2例患者以急性精神异常起病,有轻度意识障碍,而无中脑受损表现,故初诊时易与额颞叶等部位梗死混淆,亦需要与病毒性脑炎、急性应激障碍等相鉴别。双侧丘脑病损需与Wernicke脑病、Wilson病、浸润性肿瘤、中毒性疾病等鉴别。Percheron动脉太细,MRA 及传统血管造影术不能使其显影,只有超选择性血管造影术能显影,且其闭塞后无法显影,因此临床大多根据缺血部位推测其存在。该2例患者急性起病,出现精神行为异常及嗜睡,影像学证实双侧丘脑急性梗死,虽无Percheron动脉解剖变异的直接证据,但根据典型的临床表现及影像学改变诊断为Percheron动脉梗死。
栓塞为引起Percheron梗死常见发病机制,包括心源性、动脉源性或不明原因栓塞。该报道中第1例患者有房颤,第2例患者颈部血管彩超检查均存在动脉硬化斑块,分析可能通过心源性栓塞或动脉-动脉栓塞机制引起Percheron动脉梗死。基于此,有研究推荐Percheron 梗死首选抗凝及rt-PA 溶栓治疗。Percheron梗死预后一般较好。本文报道2例患者出院半年后随访,精神症状基本消失。丘脑梗死常以偏瘫、偏身感觉障碍起病,双侧丘脑梗死且以精神障碍为主要表现的病例少见,易被临床忽视。影像学检查发现,双侧丘脑梗死时应想到Percheron动脉闭塞的可能,尽早制定相应的治疗方案,并积极寻找可能存在的血栓证据。
原始出处:
李乐,余丹芳,张帆.以精神异常起病的双侧丘脑梗死2例报告[J].中国实用神经疾病杂志,2018,21(15):1733-1735.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







学习
64
非常受益,很好的研究
58
#脑梗#
35
#双侧#
27
#丘脑#
0
#丘脑#
22