Neurology : 前循环脑梗前,若存在运动障碍,预后如何?
2021-09-26 Freeman MedSci原创
https://pubmed.ncbi.nlm.nih.gov/34544817/
AHA/ASA指南建议为符合条件的缺血性卒中患者提供血管内血栓切除术(EVT),其病前修改的Rankin量表(mRS)<2.病前残疾(mRS≥2)的患者基本上被排除在关键的EVT试验之外。
然而,病前中度至重度残疾的患者,占所有缺血性卒中患者的三分之一。
此外,最近在美国进行的一项双中心研究显示,病前mRS≥2的患者占真实世界EVT病例的34%,与病前mRS 0-1的患者相比,根据mRS评分从卒中前到90天的变化,显示出与病前残疾水平相似的恢复。
之前的一项多中心观察性研究报告了类似的结果,但仅限于欧洲的中心。然而,在美国的中心,还没有进行过一项关于用EVT和第二代支架植入器治疗的病前mRS≥2的多中心研究。
为了给这样的试验提供更多的证据,需要一个前瞻性的随机临床试验来确定EVT对病前残疾患者的益处,
藉此,美国University of Utah的Adam de Havenon在一个大型的、多中心的、注册数据,研究了病前残疾对EVT后结果的影响。
他们对TREVO支架-复位器急性卒中(TRACK)登记处进行了事后分析,该登记处收集了美国23个中心使用Trevo设备作为一线EVT治疗的634名连续卒中患者的数据。
他们纳入了颈内动脉或大脑中段(M1/M2段)闭塞的患者,研究暴露为患者或护理人员报告的病前改良等级表(mRS)≥2(病前残疾,PD)与病前mRS评分0-1(无病前残疾,NPD)。
主要结果是没有累积残疾,定义为90天的mRS与患者病前的mRS相比没有增加。
在TRACK的634名患者中,407名患者被纳入我们的队列,其中53/407(13.0%)患有PD。37.7%(20/53)的PD患者和16.7%(59/354)的NPD患者达到了无累积残疾的主要结果(P<0.001),而39.6%(21/53)和14.1%(50/354)的患者发生死亡(P<0.001)。
与NPD患者相比,PD患者无累积残疾的调整后几率为5.2(95% CI 2.4-11.4,p<0.001)。然而,PD患者死亡的调整后几率为2.90(95% CI 1.38-6.09,p=0.005)。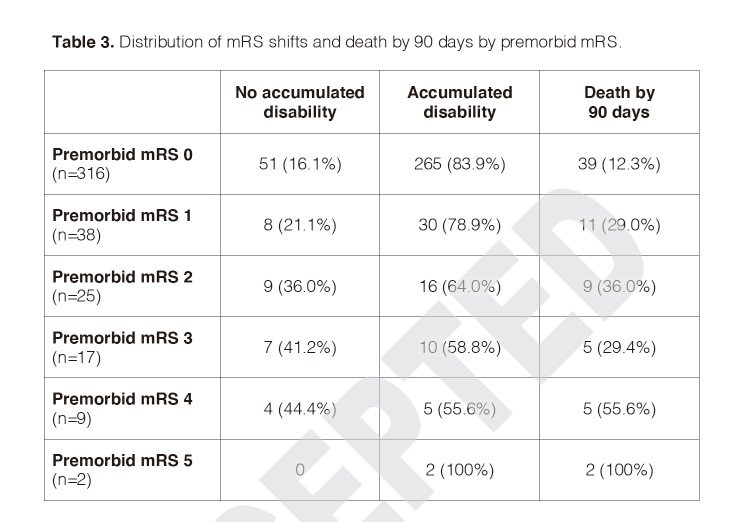
在这项对前循环急性缺血性卒中患者进行EVT治疗的研究中,他们发现,与没有前循环残疾的患者相比,前循环残疾与不积累更多残疾的概率有关,但也与更高的死亡概率有关。
原文出处:
de Havenon A, Castonguay A, Nogueira R, et al. Prestroke Disability and Outcome After Thrombectomy for Emergent Anterior Circulation Large Vessel Occlusion Stroke. Neurology. Published online September 20, 2021:10.1212/WNL.0000000000012827. doi:10.1212/WNL.0000000000012827
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Neurol#
32
#预后如何#
34
#运动障碍#
35
#脑梗#
26
学习了,不错不错
62