盘点:近期非酒精性脂肪肝重要研究进展一览
2017-08-22 MedSci MedSci原创
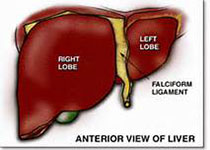
脂肪肝,是指由于各种原因引起的肝细胞内脂肪堆积过多的病变。脂肪性肝病正严重威胁国人的健康,成为仅次于病毒性肝炎的第二大肝病。脂肪肝是一种常见的临床现象,而非一种独立的疾病。其临床表现轻者无症状,重者病情凶猛。非酒精性脂肪性肝病是指除外酒精和其他明确的损肝因素所致的肝细胞内脂肪过度沉积为主要特征的临床病理综合征,与胰岛素抵抗和遗传易感性密切相关的获得性代谢应激性肝损伤。这里梅斯小编整理了近期关于非酒
脂肪肝,是指由于各种原因引起的肝细胞内脂肪堆积过多的病变。脂肪性肝病正严重威胁国人的健康,成为仅次于病毒性肝炎的第二大肝病。脂肪肝是一种常见的临床现象,而非一种独立的疾病。其临床表现轻者无症状,重者病情凶猛。非酒精性脂肪性肝病是指除外酒精和其他明确的损肝因素所致的肝细胞内脂肪过度沉积为主要特征的临床病理综合征,与胰岛素抵抗和遗传易感性密切相关的获得性代谢应激性肝损伤。这里梅斯小编整理了近期关于非酒精性脂肪性肝病的重要研究进展与大家一同分享。
【1】非酒精性脂肪肝与心血管疾病及其他肝外疾病的关系
肝脏的主要生理功能包括葡萄糖和脂质代谢,在非酒精性脂肪性肝病(NAFLD)中这些代谢功能出现紊乱,并可能与部分由肝脏分泌的细胞因子和分子引发的全身炎症“环境”有关。
大量的临床证据表明NAFLD与心血管疾病(CVD)、慢性肾脏病(CKD)和2型糖尿病(T2DM)的流行独立相关。这些肝外疾病发生的风险大小与NAFLD潜在的严重程度相关,非酒精性脂肪性肝炎(NASH)的患者相比于单纯性脂肪变性的患者发生CVD、CKD和2型糖尿病的风险似乎更大。新的数据还表明NAFLD可能是结肠肿瘤和骨密度降低的危险因素,尤其是在男性患者中。更重要的是,改善/解决NAFLD与T2DM的发病率降低和改善肾功能有关,将体重纳入到因果关系中,并建议肝为重点的治疗可能会减少肝外并发症的风险。
【2】乙肝病毒感染或对非酒精性脂肪肝病有益
乙肝和脂肪肝有没有关联?2017年3月,发表在《Hepatology》的一项由韩国科学家进行的队列研究表明,乙肝病毒感染可能对非酒精性脂肪肝病(NAFLD)进展的发病机制具有影响。
慢性乙肝病毒(HBV)感染与脂肪肝之间的相关性是有争议的。研究人员考察了HBV感染与NAFLD进展之间的相关性。研究共纳入了83339名参与者,校正年龄、性别、就诊年、吸烟状态、酒精摄入、常规锻炼、教育水平和体重指数后发现,HBsAg阳性参与者NAFLD的发病风险降低。表明HBV感染可能对NAFLD进展的发病机制具有影响。
【3】非酒精性脂肪肝患者中氨基酸水平影响肥胖和胰岛素抵抗
在非酒精性脂肪性肝病(NAFLD)中,经常发现氨基酸(AA),特别是支链(BCAA)的血浆浓度增加。然而,这一现象是否是由于增加的肌肉蛋白质分解代谢,肥胖和/或胰岛素抵抗(IR)增加或是由于受损的组织代谢导致的仍然尚未可知。新的一项研究对此进行了探究,结果显示,大多数AA仅在NAFLD-Ob人群中增加。与CT人群相比,NAFLD-NO受试者只有丙氨酸、谷氨酸、异亮氨酸和缬氨酸增加,而非亮氨酸。谷氨酸、酪氨酸和GSG指数与Hep-IR相关。GSG指数与肝酶,特别是GGT相关,而与BMI无关。肝活检中的气球样变和/或炎症与血浆BCAA和Aromatic-AA水平的增加相关,与GSG指数轻度相关,而新GSG指数在该队列中仅能区分F3-4与F0-2的纤维化。表明AA血浆浓度的增加主要在肥胖的NAFLD受试者中出现,这可能是IR和蛋白质分解代谢增加的结果。GSG指数是独立于BMI的代表肝脏疾病严重程度的新标志物。
【4】咖啡摄入量与非酒精性脂肪肝患者的亚临床CVD或CVD事件风险无关
动脉粥样硬化及其临床后遗症是导致非酒精性脂肪肝(NAFLD)患者死亡的主要原因。虽然流行病学数据支持NAFLD患者摄入咖啡具有保肝的好处,但是,咖啡是否可以改善NAFLD相关的心血管疾病的风险仍是未知的。近日,新的一项研究对此进行了探究,结果显示,NAFLD患者更容易出现BMI升高和糖尿病,但在每日摄入咖啡的患者中没有差异,在NAFLD患者中,咖啡摄入与基础CAC>0的患病率无关。在12.8年的随访中,93名NAFLD患者和415名非NAFLD参与者经历了心血管事件。然而,在NAFLD或非NAFLD者中咖啡的摄入量与心血管疾病事件发生无关。表明,咖啡摄入量与亚临床心血管病的患病率没有关系,咖啡也不会影响未来的心血管事件的风险,无论潜在的NAFLD状态如何。
【5】HMGB1-RAGE通路介导与非酒精性脂肪肝高度相关的肠道炎症
近来不少临床研究发现结肠炎症和IBD(炎症性肠病)样表型与NAFLD(非酒精性脂肪肝)高度相关,但是其中的机制仍然未知。发表于Redox Biol的一篇论文中,研究人员对其中的机制进行了研究,并且探究了此途径的氧化还原信号传导机制。结果显示HMGB1为NAFLD引起肠道炎症的关键介质,并且其介导的炎性通路具有RAGE和氧化还原信号依赖性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#酒精性脂肪肝#
0
#非酒精性#
30
#酒精性#
24
#研究进展#
30
真的很棒.希望能够继续进行盘点.作为一个科研新手.这是了解最新资讯的唯一途径了
66