JBC:科学家发现癌细胞抗氧化应激损伤的机制
2012-04-10 Beyond 生物谷
化疗和辐射引起癌细胞氧化应激,进而杀死肿瘤细胞。南加州大学的一项新的研究表明,保护癌症和其他细胞免受应激压力的一种蛋白质有一天能够帮助医生打破癌细胞的防御能力,使得癌细胞对相应治疗更敏感。 南加州大学教授Kelvin J. A. Davies率领的研究团队完成的最新研究证实蛋白质Nrf2能增强细胞应对氧化应激的能力。相关研究论文发表在3月23日的《生物化学杂志》上。 氧化应激是指体内氧化与抗氧
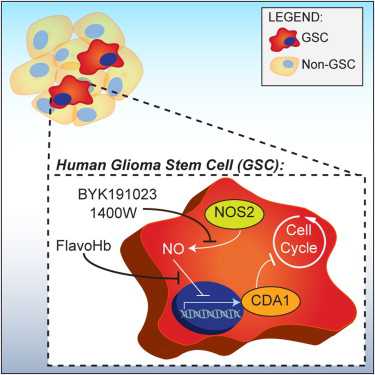
化疗和辐射引起癌细胞氧化应激,进而杀死肿瘤细胞。南加州大学的一项新的研究表明,保护癌症和其他细胞免受应激压力的一种蛋白质有一天能够帮助医生打破癌细胞的防御能力,使得癌细胞对相应治疗更敏感。
南加州大学教授Kelvin J. A. Davies率领的研究团队完成的最新研究证实蛋白质Nrf2能增强细胞应对氧化应激的能力。相关研究论文发表在3月23日的《生物化学杂志》上。
氧化应激是指体内氧化与抗氧化作用失衡,倾向于氧化,导致中性粒细胞炎性浸润,蛋白酶分泌增加,产生大量氧化中间产物。氧化应激是由自由基在体内产生的一种负面作用,并被认为是导致衰老和疾病的一个重要因素。
Davies说:“在癌细胞中,如果有一天能有选择性地关闭Nrf2蛋白,化疗和放射治疗可能会变得更有效”。
Nrf2是一种转录因子蛋白质,Davies实验室的研究工作表明在氧化应激过程中,蛋白酶和蛋白酶体调节因子(PA28)的生成是由Nrf2控制的。反过来,蛋白酶是一个大的蛋白质酶,能分解氧化的蛋白,氧化的蛋白积累的话会导致细胞死亡。
当肿瘤细胞氧化应激反应增加(实验室中用过氧化氢刺激肿瘤细胞,过氧化氢放疗和化疗过程中主要产物)时,Davies和他的团队发现细胞Nrf2会加速蛋白酶的产生。
然后研究人员通过各种化学和遗传抑制剂阻断Nrf2来测试他们的研究结果,结果发现Nrf2被抑制后,细胞生成蛋白酶以及处理双氧水的能力减弱。
在正常细胞中,Nrf2允许蛋白酶连续生成以应对不断变化的氧化环境。但这种能力随着衰老可能会下降,使年长者应对应激的能力下降。
Davies说:我们希望能够在正常细胞中扭转这种下降趋势,降低癌细胞中Nrf2的表达,使癌细胞的抗应激能力下降,更容易死于放疗和化疗。(生物谷:Bioon)

doi:10.1074/jbc.M111.277145
PMC:
PMID:
Nrf2-dependent Induction of Proteasome and Pa28αβ Regulator Are Required for Adaptation to Oxidative Stress
Andrew M. Pickering§, Robert A. Linder§, Hongqiao Zhang, Henry J. Forman and Kelvin J. A. Davies§,1
The ability to adapt to acute oxidative stress (e.g. H2O2, peroxynitrite, menadione, and paraquat) through transient alterations in gene expression is an important component of cellular defense mechanisms. We show that such adaptation includes Nrf2-dependent increases in cellular capacity to degrade oxidized proteins that are attributable to increased expression of the 20 S proteasome and the Pa28αβ (11 S) proteasome regulator. Increased cellular levels of Nrf2, translocation of Nrf2 from the cytoplasm to the nucleus, and increased binding of Nrf2 to antioxidant response elements (AREs) or electrophile response elements (EpREs) in the 5′-untranslated region of the proteasome β5 subunit gene (demonstrated by chromatin immunoprecipitation (or ChIP) assay) are shown to be necessary requirements for increased proteasome/Pa28αβ levels, and for maximal increases in proteolytic capacity and stress resistance; Nrf2 siRNA and the Nrf2 inhibitor retinoic acid both block these adaptive changes and the Nrf2 inducers dl-sulforaphane, lipoic acid, and curcumin all replicate them without oxidant exposure. The immunoproteasome is also induced during oxidative stress adaptation, contributing to overall capacity to degrade oxidized proteins and stress resistance. Two of the three immunoproteasome subunit genes, however, contain no ARE/EpRE elements, and Nrf2 inducers, inhibitors, and siRNA all have minimal effects on immunoproteasome expression during adaptation to oxidative stress. Thus, immunoproteasome appears to be (at most) minimally regulated by the Nrf2 signal transduction pathway.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JBC#
34
#科学家发现#
35
#癌细胞#
30
#损伤#
37
#应激#
31