病例介绍
主诉 心悸、多汗、怕热4个月,双眼球突出、胀痛1个月。
现病史 患者4个月余前无明显诱因出现心悸、多汗、怕热,伴有多食、大便次数增多,每日大便4~5次,为成形软便,于当地医院检查心电图示:窦性心动过速,给予盐酸普萘洛尔控制心率,症状无好转。1个月前开始出现双眼球突出、胀痛,伴有复视、怕光,查甲状腺功能:FT3>30p mol/L,FT4>75p mol/L,TSH <0.01μI U/ml,TPOAb 1 300U/ml,TGAb 600U/ml,开始应用甲巯咪唑,1次10mg,1日3次,治疗甲亢。治疗1个月,患者眼球突出胀痛不仅无好转,还有发展趋势,以Graves病、Graves眼病收住院治疗。
患者自发病以来精神、睡眠差,近半年来体重下降约10kg,小便正常,无夜尿增多,无尿频、尿急、尿痛,无头晕、头痛,无咳嗽、咳痰。
家族史 家族中无甲状腺疾病患者,无家族性遗传病及传染病史。
个人史 无烟、酒等不良嗜好。
既往用药史 入院前曾行药物治疗,具体品种有甲巯咪唑、盐酸普萘洛尔。
过敏史 无药物及食物过敏史。
【体格检查】
一般状况 女性,52岁,身高156c m,体重48kg,发育正常,营养欠佳,体质消瘦。神清语利,查体合作。
生命体征 T 37﹒1℃,P 120次/分,R 20次/分,BP 126/60 mmHg。
皮肤 全身皮肤黏膜无黄染,无皮下出血、皮疹,无肝掌及蜘蛛痣。全身浅表淋巴结未及肿大。
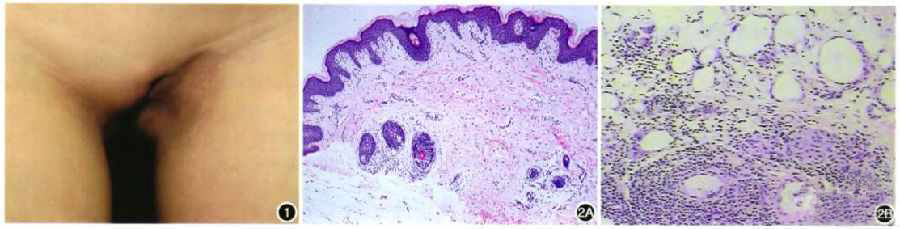
五官 头颅无畸形,眼睑轻度水肿,眼球突出,球结膜充血水肿,巩膜无黄染,双侧瞳孔正大等圆,直径约3mm,对光反射灵敏。耳鼻检查无异常。口唇无发绀,伸舌居中。咽无充血,扁桃体无肿大。
颈部 颈软,气管居中,甲状腺Ⅱ度肿大,质地中等,无触痛,两叶上级可闻及血管杂音。无颈静脉怒张及颈动脉异常搏动,未触及肿大淋巴结。
胸部 胸廓对称,无畸形,双侧呼吸动度对称,语颤正常,叩诊清音,双肺呼吸音稍粗,可闻及干性啰音。
心脏 心前区无隆起,剑突下可见心脏搏动,未触及震颤,叩心界不大,心率120次/分,第一心音增强,各瓣膜区未闻及杂音。
腹部 舟状腹,腹软,无压痛、反跳痛及肌紧张,肝于肋缘下1c m,边缘锐利,质软,无触痛,脾肋下未及。叩诊鼓音,移动性浊音阴性。双肾区无叩击痛,肠鸣音正常存在。
四肢 脊柱、四肢关节无畸形,肌力肌张力正常,双下肢无水肿。
神经系统 生理反射存在,双巴氏征阴性。脑膜刺激征阴性。
辅助检查
1﹒甲状腺功能 FT322﹒08p mol/L ↑,FT452﹒14p mol/L ↑,TSH <0.01μIU/ml,TPOAb>1 300U/ml ↑,TGAb 500U/ml ↑。
2﹒肝功能 TBIL 69﹒0μmol/L ↑,IBIL 35﹒90μmol/L ↑,DBIL 33﹒10μmol/L ↑,ALT 15﹒0U/L,AST 45﹒0U/L ↑。
3﹒血常规 WBC 4﹒9 ×109/L,NEUT 2﹒8 ×109/L,RBC 3﹒6 ×1012/L,HGB 103g/L ↓,PLT 78×109/L ↓。
4﹒空腹血糖4.1mmol/L,HbA1c 6﹒1%。
5﹒肾功能 BUN 5﹒0 mmol/L,Crea 68﹒3μmol/L。
6﹒血脂 CH OL 2﹒23mmol/L ↓,TG 0﹒43mmol/L,HDL 0﹒74 mmol/L ↓,LDL 1﹒29mmol/L。
7﹒电解质 Na 144﹒0mmol/L,K 3﹒36mmol/L ↓,Ca 2﹒09mmol/L ↓,Phos 1﹒17mmol/L,Mg 0﹒56mmol/L ↓。
8﹒心电图 窦性心动过速(120次/分);Ⅱ、Ⅲ、avF、V5~V6导联T波低平。
9﹒胸片 心肺膈未见异常。
10﹒甲状腺超声 甲状腺体积饱满,弥漫性病变,血流丰富。
11﹒心脏超声 双房扩大,退行性瓣膜病,EF 60﹒42%。
入院诊断 Graves病,甲亢:①甲亢眼病;②肝功能损伤。
维生素B1片20mg tid po
甲巯咪唑片10mg tid po
酒石酸美托洛尔片25mg tid po
甘草酸二铵肠溶胶囊100mg tid po
注射用肝水解肽100mg+10%氯化钾注射液5ml +生物合成人胰岛素注射液3U +5%葡萄糖注射液250ml ivgtt qd
注射用甲基泼尼松龙1 000mg +0.9%氯化钠注射液100ml ivgtt qd
患者入院后,根据典型的症状及化验检查,Graves病、甲状腺功能亢进症、甲亢眼病诊断明确,但患者已经应用抗甲状腺药物治疗了1个月,目前存在肝功能异常,追问患者,在应用甲巯咪唑之前没有检查血常规和肝功能,所以尚不能确定肝功能损伤的原因是甲亢所致,还是抗甲状腺药物引起,还是有肝胆系统的原发疾病,故继续应用甲巯咪唑,同时保肝降低黄疸指数治疗,并做乙肝五项、肝胆B超除外肝胆疾患。因为患者有突眼,根据《中国甲状腺疾病诊治指南》对患者的突眼进行了临床活动评分(CAS),CAS为4分,超过了3分,判断为疾病活动,所以采用了大剂量糖皮质激素冲击治疗,连续冲击治疗3天后改为泼尼松50mg/d口服。治疗期间复查肝功能,TBIL 26﹒80μmol/L ↑,IBIL 13﹒70μmol/L ↑,DBIL 13﹒10μmol/L,ALT 29﹒0U/L,AST 32﹒0U/L,明显好转,患者乙肝五项均阴性,肝胆超声未见异常,因此考虑肝功能异常是甲亢本身引起,故继续给予抗甲状腺药物(甲巯咪唑片)治疗。密切监测血常规及肝功能的变化。患者于住院期间出现咳嗽、咳痰,偶有喘憋,活动后不明显,考虑患者由于甲亢消耗多、体质差,加之大剂量激素冲击治疗,患者的抗感染能力明显下降,出现了院内感染,给予头孢呋辛抗感染治疗同时给予盐酸氨溴索雾化化痰治疗。住院20余天后复查甲状腺功能:FT314﹒88p mol/L,FT431﹒6p mol/L,TSH 0﹒045μI U/ml,心悸、怕热、多汗症状较前改善,尤其是眼睛胀痛明显减轻,眼睑和结膜水肿消失,无咳嗽、咳痰,出院。
出院诊断
1﹒Graves病,甲亢 ①甲亢眼病;②肝功能损伤。
2﹒上呼吸道感染。
病例特点与诊断要点
1﹒病史
患者4个月前出现心悸、多汗、怕热,大便次数增多等甲亢症状,1个月前出现了双眼球突出、胀痛伴怕光、流泪。
2﹒甲状腺功能
FT322﹒08p mol/L ↑,FT452﹒14p mol/L ↑,TSH < 0﹒01μI U/ml,TPOAb >1 300U/ml ↑,TGAb 500U/ml ↑。
3﹒肝功能
TBIL 69﹒0μmol/L ↑,IBIL 35﹒90μmol/L ↑,DBIL 33﹒10μmol/L ↑,ALT 15﹒0U/L,AST 45﹒0U/L↑。
4﹒血常规
WBC 4﹒9 ×109/L ↓,NEUT 2﹒8 ×109/L ↓,RBC 3﹒6 ×1012/L,HGB103g/L ↓,PLT 78×109/L ↓。
5﹒甲状腺超声
甲状腺体积饱满,弥漫性病变,血流丰富。
用药分析与药学监护
1﹒抗甲状腺药物
常用的抗甲状腺药物主要有硫脲类和咪唑类两种,都可以抑制甲状腺激素的合成。甲巯咪唑(MMI)属于咪唑类,应用过程中可以对肝脏造成损伤,主要表现为胆汁淤积,造成黄疸指数升高,而甲亢本身也可以造成肝脏损伤,或表现为转氨酶升高,或表现为黄疸指数升高,区别上述两种原因造成肝损伤的重要参照标准是服用甲巯咪唑前的肝功能情况,该患者用甲巯咪唑之前未检查肝功能,对临床判断肝损伤原因增加了难度,但在保肝治疗基础上,继续应用甲巯咪唑,严密监测肝功能变化,肝功能没有恶化,并且明显好转,支持甲亢本身造成的肝损伤,所以继续采用了甲巯咪唑治疗甲亢,而没有选用丙硫氧嘧啶(虽然该药不易造成胆汁淤积,但有造成肝衰竭的报道),也没有选择手术和放射性碘治疗(均有可能加重突眼)。因为甲巯咪唑还可以造成白细胞的下降,所以治疗甲亢时要定期监测血常规的变化,尤其是治疗的前2个月。根据患者情况,权衡利弊,选择了MMI治疗。
抗甲状腺药物治疗时应注意监护:①血常规监测:由于抗甲状腺药物本身可以引起粒细胞减少,甚至可见粒细胞缺乏,一般发生在用药后2~3个月,但也可见于任何时间,所以应密切监测血常规变化,如果粒细胞明显减少,或者出现咽痛、发热等症状时,则需立即停药,并且给予对症处理;②肝功能监测:抗甲状腺药物可以引起肝功能异常、黄疸、肝大、肝坏死、肝细胞损害和胆汁淤积型肝炎等,患者应用抗甲状腺药物之前胆红素明显升高,在保肝的同时加用此药,应动态监测其变化趋势。
2﹒糖皮质激素
Graves眼病是一种常见的与甲状腺相关的器官特异性自身免疫病。主要表现为眼睑挛缩、眼球突出、球结膜水肿、眶周水肿以及眼球活动障碍,严重者可出现角膜暴露、复视,以及可致失明的压迫性视神经病变。Graves眼病是甲亢治疗中的一个难题,没有特效方法。目前认为静脉激素冲击治疗是活动性甲亢眼病患者首选的治疗方法。《糖皮质激素类药物临床应用指导原则》中规定:①轻度Graves眼病:以控制甲亢或甲减为主,同时予以局部治疗,并戒烟或避免被动吸烟,注意用眼卫生,其使用糖皮质激素的风险大于疗效,可观察病情发展,如进行性加重可考虑糖皮质激素治疗;②中重度Graves眼病:中重度患者如处于活动期者(活动性评分≥3分)经典治疗方案以静脉或口服糖皮质激素治疗为主,亦可联合眶部放疗。处于非活动期(活动性评分<3分)如病情长期稳定可行康复手术;③威胁视力的Graves眼病:多因甲状腺疾病相关视神经病和(或)角膜损伤所致,需立即治疗。糖皮质激素治疗与眶内减压手术是治疗甲状腺疾病相关视神经病的有效方法,但若糖皮质激素治疗1~2周后仍未显效或出现明显副作用,应及时行眶内减压手术。
糖皮质激素可口服或静脉给药。①口服给药:可选泼尼松(龙)或相当剂量的甲泼尼龙,泼尼松起始剂量为1日80~100mg,48小时即可改善,剂量维持2~8周后逐渐减量,糖皮质激素治疗一般需维持3个月,此时加用环孢素。若处于活动期的Graves眼病患者需131I治疗,应预防性应用糖皮质激素,即131I治疗后1~3日予以泼尼松0.3~0.5mg/(kg ·d)口服,逐渐减量,2个月后停药;②静脉给药:可给予甲泼尼龙500mg,48小时可重复。重症患者可予以甲泼尼龙500~1 000mg静脉滴注冲击治疗,隔日1次,连用3次。但甲泼尼龙可因剂量累积而引起严重中毒性肝损伤甚或死亡。该患者处于Graves眼病活动期,所以采用了糖皮质激素大量冲击治疗,之后改为口服治疗长时间维持(3~12个月)。
长期大量应用糖皮质激素会引起皮质醇增多症、类固醇性糖尿病、骨质疏松、并发或者加重感染、诱发或者加重溃疡、诱发精神症状等。长期应用应补充钙剂,密切监测血糖变化,且应缓慢减药,避免出现激素停用后综合征等病情加重或反复。
3﹒控制甲亢症状治疗
甲亢时甲状腺激素分泌过多,患者的交感神经处于兴奋状态,儿茶酚胺分泌并不增多,但是对儿茶酚胺敏感的β肾上腺素受体数量上调,故有心动过速、心悸、出汗多、焦虑等症状,应用普萘洛尔后上述症状可以得到控制,此药也可以抑制外周组织的T4向T3转换。但是盐酸普萘洛尔在合并心功能不全者慎用,并且此药也可以引起白细胞减低,根据患者的状况选择酒石酸美托洛尔以控制患者交感兴奋症状。β受体阻断剂可能会引起心动过缓,故用药期间应密切监测心电图,了解其动态变化,根据结果及时调整药物剂量。
4﹒保肝治疗
甲亢本身可以造成肝功能异常,抗甲状腺药物也可损伤肝功能,因此需要在治疗过程中严密监测肝功能变化,该患者已经出现了肝功能异常,所以给予了保肝治疗。甘草酸二铵肠溶胶囊具有较强的抗感染、保护肝细胞膜及改善肝功能的作用,亦能明显减轻D‐氨基半乳糖对肝脏的形态损伤和改善免疫因子对肝脏形态的慢性损伤。肝水解肽能促进蛋白质合成,减少蛋白质分解,促进正常肝细胞的增殖和再生。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Graves#
31
#肝功能#
26
#损伤#
21
#Graves病#
44
#眼病#
41
陈vvvv不会后悔
47
学习一下谢谢
53
古古怪怪沟沟壑壑
52