中国循环杂志:这些高危患者搭桥术前或需应用IABP
2017-04-25 佚名 中国循环杂志
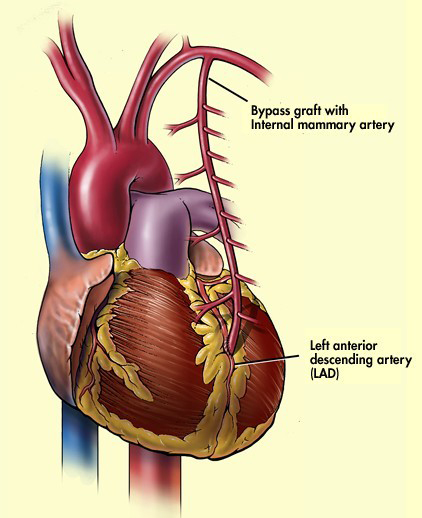
对于手术危险较高的搭桥患者,围手术期常需主动脉内球囊反博(IABP)进行辅助支持。近期阜外医院王现强、王巍、王跃堂等进行的研究显示,对于高危搭桥患者,术前置入IABP优化短期预后,而再次置入IABP是短期死亡的危险因素。 其中高危冠心病的诊断标准为:(1)≥3支冠脉显著狭窄;(2)冠脉左主干显著狭窄;(3)LVEF<0.4,或NYHA分级III 级或者IV 级;(4)急性心肌梗死或者药物
对于手术危险较高的搭桥患者,围手术期常需主动脉内球囊反博(IABP)进行辅助支持。近期阜外医院王现强、王巍、王跃堂等进行的研究显示,对于高危搭桥患者,术前置入IABP优化短期预后,而再次置入IABP是短期死亡的危险因素。
其中高危冠心病的诊断标准为:(1)≥3支冠脉显著狭窄;(2)冠脉左主干显著狭窄;(3)LVEF<0.4,或NYHA分级III 级或者IV 级;(4)急性心肌梗死或者药物难以控制的不稳定性心绞痛;(5)Euro SCORE ≥ 6 分。
研究显示,与术后置入IABP的患者相比,术前置入组在术后48 h时,心肌酶峰值明显降低,机械通气时间和总住院时间显著减少。
而且,急性肾损伤、脑并发症和术后30天死亡率的发生率均显著降低,中位生存时间显著延长。
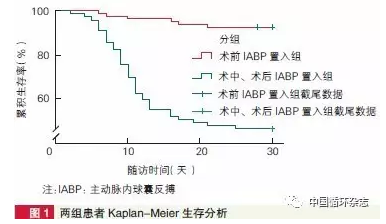
该研究共纳入应用IABP辅助的197例高危冠心病搭桥患者,其中男性占46.2%,有89例术前置入IABP,108例为术后置入,两组人群基线特征无显著差异。
原始出处:王跃堂, 丘俊涛, 王旭, 等. 主动脉内球囊反搏置入时机对高危冠心病患者行冠状动脉旁路移植术的短期效果评价和危险因素分析. 中国循环杂志, 2017, 32: 232-236.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#高危患者#
21
#ABP#
23
#搭桥#
24
#搭桥术#
34
#IABP#
31
临床上感觉也是这样
45
继续关注。
50