Nature Medicine: 发现一型胰岛素突变引起1型糖尿病病
2017-05-01 MedSci MedSci原创
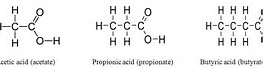
这项研究发现了临床中存在的一种新的来自非正常翻译而产生的突变型胰岛素蛋白,并且揭示其足以能够作为自身T细胞的抗原,从而介导杀死胰岛的β细胞,引起1型糖尿病。这一新抗原的发现,作为未来开发中和抗体,为抑制T细胞免疫的反生,提供了理论基础。未来可以因此,筛选含有这一基因突变的1型糖尿病病人,而对此采取个性化疗法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胰岛素突变#
31
#CIN#
32
#胰岛#
39
#DIC#
41
#Nat#
30
学习了,谢谢
77
不错的方式,努力学习,刻苦专研,不断总结出来新经验。给点个赞!
2
一种新鲜的假设
63
#Med#
28
#Medicine#
26