J Hepatol:超米兰标准中期多发性肝癌患者 肝切除术优于介入治疗
2014-07-25 MedSci MedSci原创
新一期国际权威期刊《肝病学杂志》发布了第二军医大学东方肝胆外科医院周伟平教授等人的科研成果。他们为期3年的随机对照临床研究表明:对于超米兰标准的中期多发性肝癌患者,应用肝切除术治疗能提高生存率,效果显著好于介入治疗。这颠覆了欧洲肝脏研究学会推荐的巴塞罗那指南,即中期肝癌患者最佳的治疗方案是介入——而这一共识自1999年以来基本未变。【小知识】米兰标准:世界上应用最广泛的标准,具体是指单个肿瘤直径
近期在 J Hepatol 发布了一篇颠覆性研究结果。第二军医大学东方肝胆外科医院周伟平教授等人的最新科研成果表明:肝切除术能显著提高超米兰标准的中期多发性肝癌患者的整体生存率。
这一研究成果则挑战了欧洲肝脏研究学会(European Association for the Study of the Liver)推荐的指南:中期肝癌患者的最佳治疗方案是介入——而这一共识是基于1999年一项临床研究。
研究方法:

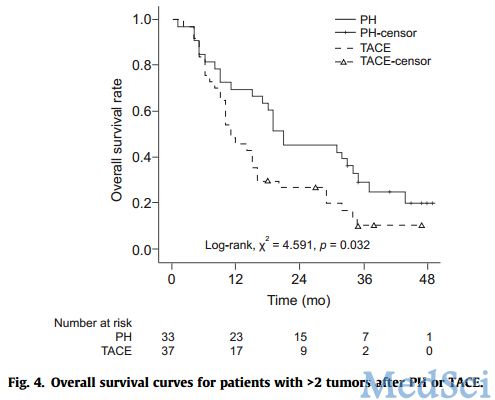
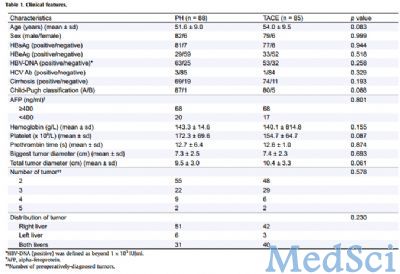
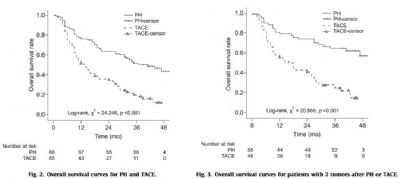
对这173例患者后进行生存分析显示,第1、2、3年PH组总生存率分别为76.1%,63.5%和51.5%,TACE组分别为51.8%,34.8%和18.1%。PH组疗效明显好于TACE组,两组患者的中位生存时间分别为41个月和14个月,接受肝切除治疗的患者肝癌相关死亡风险降低56.6%。(图2、3)
研究显示,在谨慎选择合适的肝癌患者基础上,对于超米兰标准的中期多发性肝癌患者,肝切除相对于介入治疗可显著提高肝癌患者生存率。
原始出处:
Yin L1, Li H2, Li AJ1, Lau WY3, Pan ZY1, Lai EC3, Wu MC1, Zhou WP4.Partial hepatectomy vs. transcatheter arterial chemoembolization for resectable multiple hepatocellular carcinoma beyond Milan criteria: A RCT.J Hepatol. 2014 Jul;61(1):82-8. doi: 10.1016/j.jhep.2014.03.012. Epub 2014 Mar 17.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
32
#多发性#
26
#肝切除#
32
是滴是滴,显然直接切的好咯
127
#肝癌患者#
36
#肝切除术#
44
#EPA#
31