JCI:上海交通大学刘芳团队揭示抑郁症脱髓鞘化分子机制
2022-04-21 周科 “神经周K”公众号
酪氨酸蛋白激酶A4受体 (EphA4) 是酪氨酸蛋白激酶家族成员,是神经元突触后膜的重要细胞表面受体。
 轴突髓鞘形成维持中枢神经系统的电活动功能至关重要。髓磷富含髓磷脂碱性蛋白(MBP)、蛋白脂质蛋白和环核苷酸磷酸二酯酶等多种多种髓磷脂特异性蛋白质。多发性硬化症存在典型的脱髓鞘病变。抑郁症患者与多发性硬化症存在很高的共患病率。抑郁症患者脑组织少突胶质细胞密度降低,相关基因表达也减少。
轴突髓鞘形成维持中枢神经系统的电活动功能至关重要。髓磷富含髓磷脂碱性蛋白(MBP)、蛋白脂质蛋白和环核苷酸磷酸二酯酶等多种多种髓磷脂特异性蛋白质。多发性硬化症存在典型的脱髓鞘病变。抑郁症患者与多发性硬化症存在很高的共患病率。抑郁症患者脑组织少突胶质细胞密度降低,相关基因表达也减少。
酪氨酸蛋白激酶A4受体 (EphA4) 是酪氨酸蛋白激酶家族成员,是神经元突触后膜的重要细胞表面受体。EphA4的激活引起中枢神经系统和外周神经系统髓鞘的形成。EphA4 主要在成年海马中表达,可抑制神经传递和突触可塑性。多发性硬化症和脑损伤中EphA4表达增加。
2022年4月15日上海交通大学、加拿大多伦多大学精神病学系、生理学系刘芳教授研究团队在The Journal of Clinical Investigation杂志发表文章揭示了EphA4在抑郁症脱髓鞘化中发挥关键作用。
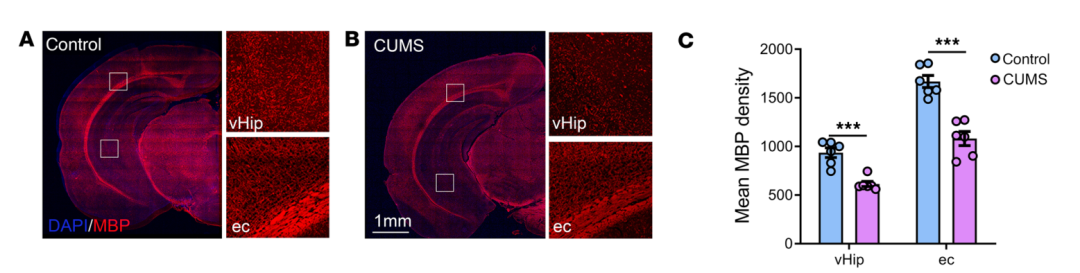
图1:抑郁症动物模型出现脱髓鞘化
慢性不可预见性动物应激模型(CUMS)和脂多糖(LPS)可引起小鼠抑郁样行为。研究人员通过免疫荧光实验和分子学实验发现CUMS和LPS引起的抑郁样小鼠中腹侧海马MBP水平明显降低,存在脱髓鞘化,突触蛋白表达也减少。
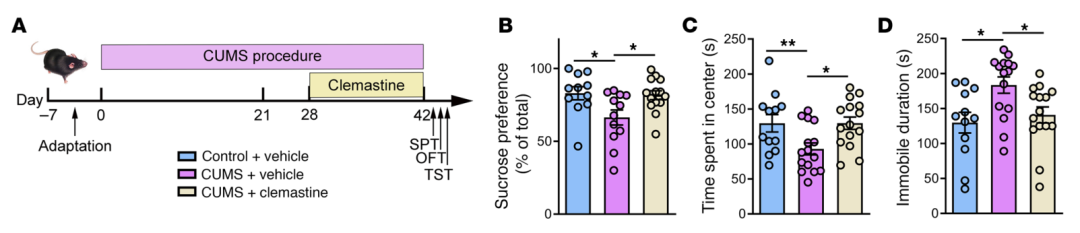
图2:Clemastine处理可改善抑郁样行为
Clemastine在多发性硬化症患者和动物模型中具有促进髓鞘再生作用。连续给与2周Clemastine后能够明显改善慢性应激引起的抑郁样行为,增加海马区域MBP蛋白的表达。这一改善也出现在脂多糖引起的抑郁症模型中。
慢性应激引起海马突触密度降低,突触后致密区域厚度减小,在给予Clemastine后能够增加该区域突触密度,增加突触后致密区域的厚度,这就表明该药物能够逆转慢性应激引起的海马区域突触结构障碍和脱髓鞘改变。
进一步通过分子实验发现慢性应激或LPS引起的抑郁样小鼠海马区域Epha4蛋白表达增加。蛋白质谱分析发现慢性应激过程中与Epha4蛋白存在互相作用的蛋白为463种,其中大多数为泛素介导的蛋白质降解信号通路。
慢性应激引起海马组织泛素化水平降低,Epha4蛋白泛素化水平也降低,这就表明慢性应激引起大脑蛋白质泛素化水平降低,促进Epha4蛋白水平。通过病毒特异性敲低海马区域Epha4后能够逆转慢性应激引起的突触结构功能和脱髓鞘功能,并改善抑郁样行为。
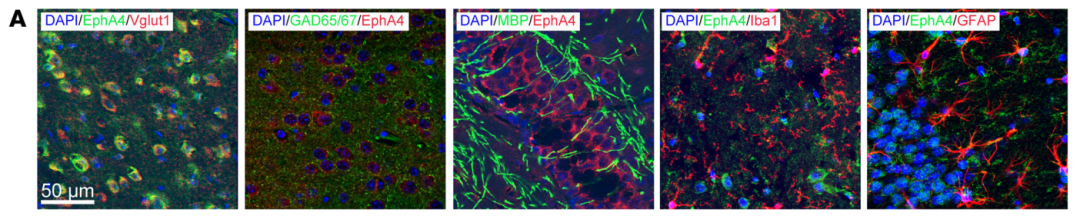
图3:Epha4主要表达在兴奋性神经元
免疫荧光实验发现Epha4主要表达在兴奋性神经元上,不表达在抑制性神经元、髓鞘、小胶质细胞和星形胶质细胞上。慢性应激促进兴奋性神经元Epha4的表达,特异性敲低该类型神经元Epha4后也能够发挥明显的抗抑郁作用。
另一方面,研究人员利用抑郁症患者组织样本发现突触蛋白、MBP水平均降低,Epha4蛋白水平,这就表明通过抑制Epha4水平或促进髓鞘再生可能发挥抗抑郁作用。
尽管之前已有研究表明海马脑区Epha4蛋白水平参与慢性应激引起抑郁样行为,但具体机制未知。本文发现Epha4蛋白通过参与应激引起的脱髓鞘化过程调控抑郁样行为。
原始出处:
Yuan Li, et al. The Eph receptor A4 plays a role in demyelination and depression-related behavior. The Journal of Clinical Investigation, 2022;132(8):e152187,https://doi.org/10.1172/JCI152187.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCI#
28
#髓鞘#
28
#抑郁#症#脱髓鞘化#
78
#脱髓鞘#
32
#交通#
38