FICC 2014:曹秋梅谈低钠血症的诊治
2014-04-14 小田 整理 医学论坛网
第八届北京五洲国际心血管病会议(FICC2014)的中法急诊危重症论坛上,首都医科大学附属北京同仁医院曹秋梅医师介绍了低钠血症的诊治。 诊断 &
第八届北京五洲国际心血管病会议(FICC 2014)的中法急诊危重症论坛上,首都医科大学附属北京同仁医院曹秋梅医师介绍了低钠血症的诊治。
诊断
众所周知,低钠血症是指血清中钠(Na+)浓度<135 mmol/L,伴或不伴细胞外液容量改变,是临床上最常见的电解质紊乱,引起低钠血症的病因繁多。临床上,Na+<134 mmol/L的患病率为15%,Na+<125 mmol/L的患病率为5%。急性严重的低钠血症可导致极高的病死率,而过快纠正慢性低钠血症可导致严重的神经系统并发症,甚至死亡。
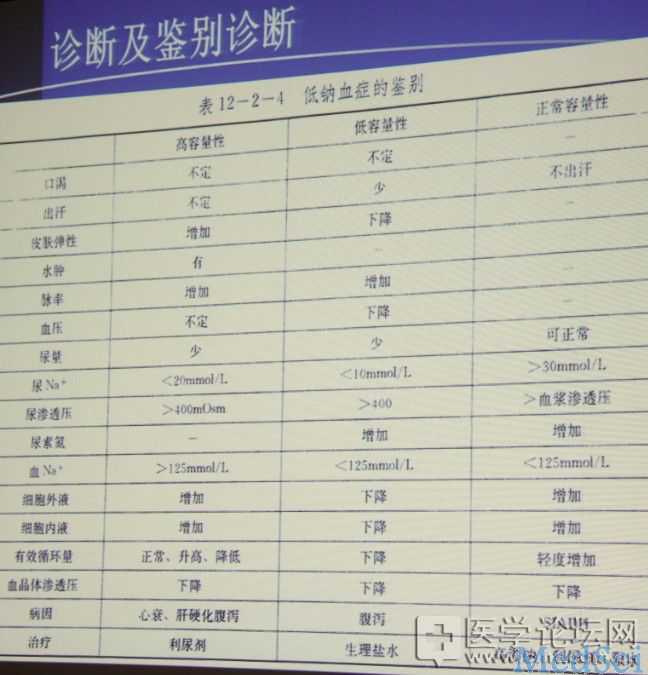
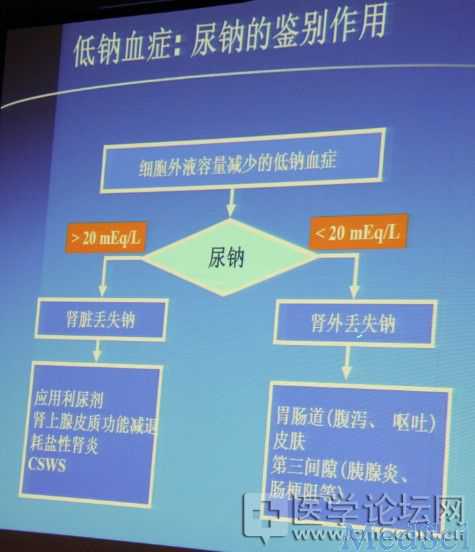
低钠血症根据血浆渗透压可分为高渗性低钠血症(异位性低钠血症)、等渗性低钠血症(假性低钠血症)和低渗性低钠血症,其中低渗性低钠血症最常见,原因为水潴留异常或水摄取过多,分为肾性和肾外性失钠,检测尿钠可行鉴别。在行低钠血症的诊断时,除外要评估患者血钠浓度、血浆渗透压浓度和尿钠以外,还应进行容量状态的评估。
根据血钠下降的速度,还可将低钠血症分为急性低钠血症和慢性低钠血症。前者是指当血钠在48小时内迅速下降至120 mmol/L以下或血钠降低<0.5 mmol/h,造成严重症状性低钠血症;后者是指当血钠在48小时或以上缓慢下降或血钠降低>0.5 mmol/h,即为慢性低钠血症,易发生渗透性脱髓鞘病变。
治疗

一、急性低钠血症的治疗
当患者血钠<110—115 mmol/L并伴有明显神经系统症状时应作紧急治疗,具体步骤如下:
第一步:6小时内使血钠升高近10 mmol或升高至120—125mmol(每小时使血钠升高1—2 mmol/L);
第二步:在随后的24—48小时或更长时间,使患者血钠浓度逐渐恢复正常。
二、慢性低钠血症的治疗
对慢性无症状性低钠血症,可对因治疗、同时限水或补充低钠溶液;对慢性有症状性低钠血症,补钠和袢利尿剂增加自由水的排泄(每小时使血钠升高1 mmol/L)。
失钠性低钠血症的治疗方法主要是补钠,同时恢复血容量。
稀释性低钠血症主要是以限水和利尿为治疗措施。
补钠注意要点
1、去除病因可使缺钠和缺水得到更快的纠正;
2、第一个24小时以内,先补缺钠量的1/3—1/2,然后根据血压、皮肤弹性、神志和尿钠浓度等补给剩余量;
3、 血浆钠离子浓度不能反映总体钠的丢失;
4、 如同时有缺钾,则须同时补给;
5、为避免过多Cl-输入,可在部分等渗液中加入1/6M乳酸钠或碳酸氢钠,如患者已发生循环衰竭,则提示缺钠严重,除外给予盐水以外,应及时补给胶体溶液;不可单独用升压药或血管扩张剂。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#低钠血症#
41
#ICC#
26
#低钠#
40