肺动脉高压的代谢、线粒体功能障碍
2022-03-08 刘少飞 MedSci原创
肺动脉高压 (PH) 代表一组以平均肺动脉 (PA) 压力升高、进行性右心室衰竭和经常死亡为特征的疾病。这种PA平滑肌细胞的过度增殖最近与代谢和线粒体生物学的变化有关,包括糖酵解、氧化还原稳态的变化。
肺动脉高压 (PH) 代表了无数以平均肺动脉压升高为特征的疾病。肺动脉高压是一种进行性的疾病,分为五个临床分类或组,取决于潜在的病因。在 I 组肺动脉高压 (PAH) 中,通常会遇到不同程度的肺血管收缩和血管重塑。标准治疗针对不同的途径来增加血管舒张。尽管有这些治疗干预,但预后通常很差,需要进一步研究上述血管重塑的发病机制,以改进新的治疗策略。血管重塑部分归因于血管驻留细胞(例如内皮细胞和平滑肌细胞)对细胞凋亡和不受控制的增殖的抵抗,以及基质沉积。导致肺血管重塑的一个新兴因素是线粒体功能障碍和代谢紊乱。本节旨在分析目前对线粒体功能障碍在 PH 发展中的作用的认识。这将包括电子传递链 (ETC) 功能障碍和能量产生从线粒体氧化磷酸化转变为糖酵解、线粒体 DNA 损伤、质量控制受损(生物发生和线粒体自噬)。对这种疾病中线粒体代谢、分子和生理作用的前沿理解应该能够开发线粒体靶向疗法,以减缓或逆转 PH 的发展。
肺动脉高压中细胞的糖酵解增强
对细胞凋亡的抵抗和肺动脉平滑肌细胞 (PASMCs) 的不受调节的过度增殖有助于肺血管重塑。这种重塑源于 PASMC 的存活和增殖增加,与线粒体代谢的变化有关,更具体地说,是从氧化磷酸化到糖酵解的转变,这一过程也称为 Warburg 效应或糖酵解开关。Warburg 效应在肿瘤发生中得到了很好的描述,它提供能量和亚状态以使肿瘤细胞快速生长。已经假设糖酵解开关的几个可能的优点。首先,糖酵解速率和葡萄糖转化为乳酸的速度加快,导致三磷酸腺苷 (ATP) 生成速度更快,但产量仍然很低。除了产生 ATP 之外,糖酵解还允许形成重要的中间分子,这些分子对于大分子的合成和促进戊糖磷酸途径 (PPP) 以及因此细胞增殖至关重要。最后,糖酵解过程中 NADPH 产量增加导致谷胱甘肽增加,这与化学抗性有关,通过其与药物的相互作用、防止 DNA 损伤以及与 ROS 的反应。在肺动脉高压中看到的代谢变化和糖酵解转变被认为类似于癌症生物学中的 Warburg 效应。
线粒体质量控制
负责线粒体质量控制的过程确保了健康的线粒体功能和细胞生物能量学。这些过程包括蛋白质稳态、生物发生、动力学(裂变和融合)和线粒体自噬。Proteostasis 是指维持正常的蛋白质折叠和结构,这是正常蛋白质定位和功能的关键。生物发生与线粒体生长和分裂的控制有关。裂变(一个线粒体分裂成两个的过程)和融合(将两个线粒体连接成一个)是线粒体动力学的核心。最后,线粒体自噬是指通过自噬去除线粒体的过程。在 PH 模型中发现了一系列线粒体质量控制的中断。
核和线粒体 DNA 损伤和肺动脉高压
DNA 的结构完整性可能会因暴露于细胞代谢物和外源性物质而受损。DNA 序列可以通过复制过程中的聚合酶破坏或环境原因(如诱变化学物质、氧化应激、辐射和慢性炎症)而改变。这些变化可以从单一碱基变化到复杂的结构变化。根据 DNA 损伤的类型,刺激相关的 DNA 损伤反应 (DDR) 途径。这些反应旨在恢复 DNA 双链体,防止受损核 DNA 的传递,并在损伤不可修复时启动细胞凋亡信号传导。
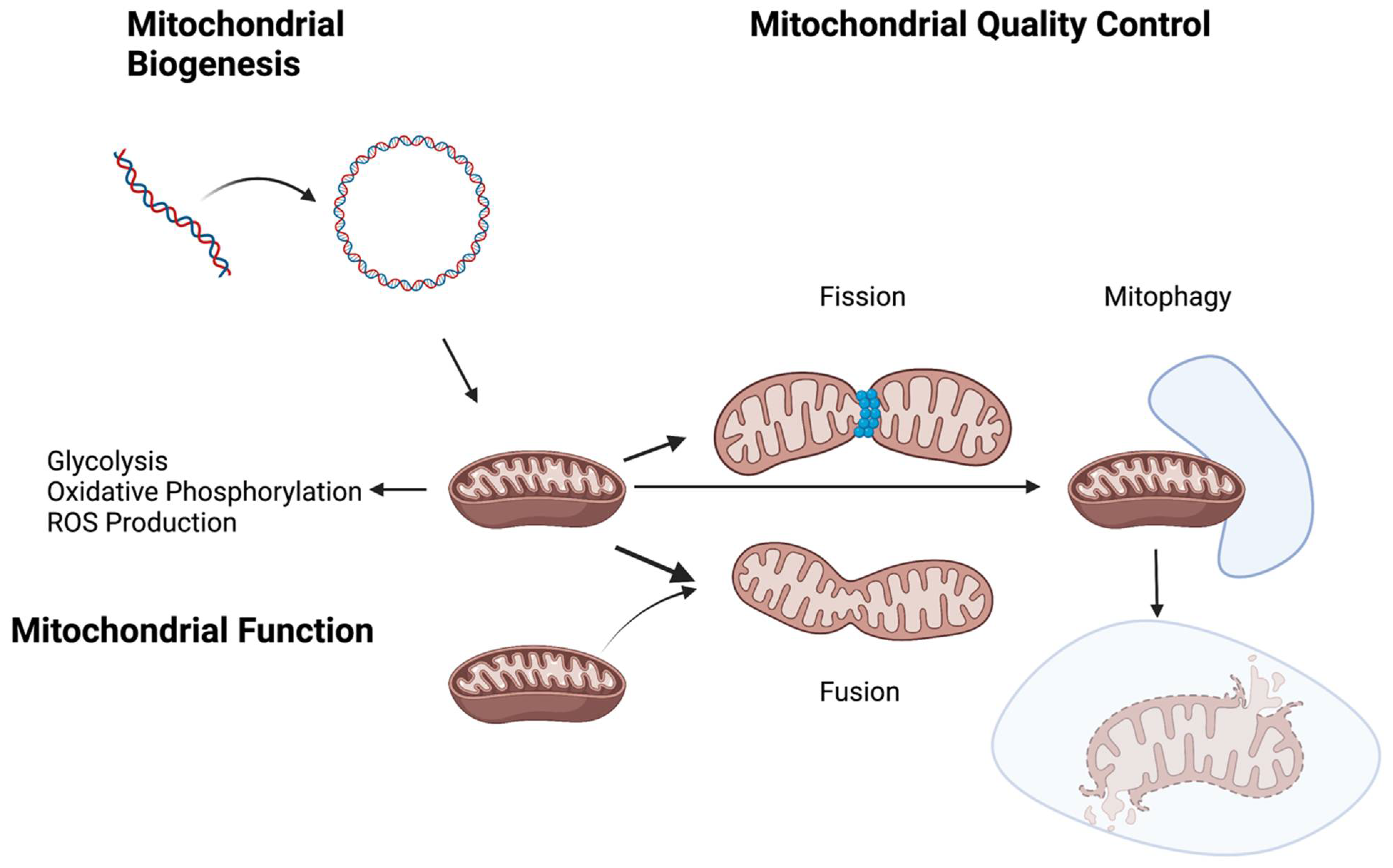
图 1. 对几种代谢和/或线粒体过程的破坏,例如糖酵解开关和氧化磷酸化,以及线粒体生物发生和质量控制的变化,与肺动脉高压的发展有关。
总之,在细胞培养、小鼠模型和 HPASMCs 中,代谢、ROS 稳态和线粒体质量控制方面都有充分的记录变化(图 1)。与癌症生物学类似,Warburg 效应或糖酵解开关已在肺动脉平滑肌细胞中得到充分描述,因为它会导致过度增殖。此外,先前在文献中也报道了线粒体生物发生和动力学的失调。其他促成因素,例如线粒体自噬和 ROS 产生的作用,仍然不确定,因为已经描述了相互矛盾的结果。随着分子技术的进步,这些争议可能会得到解决,并且可能会在 PH 中常见的不同主要分子异常之间找到联系。进一步的研究可以帮助阐明可能在这些相互作用中发挥关键作用的潜在信号分子,从而为 PH 患者提供进一步的治疗靶点候选者。
参考文献:
Colon Hidalgo D, Elajaili H, Suliman H, George MP, Delaney C, Nozik E. Metabolism, Mitochondrial Dysfunction, and Redox Homeostasis in Pulmonary Hypertension. Antioxidants (Basel). 2022 Feb 21;11(2):428. doi: 10.3390/antiox11020428. PMID: 35204311; PMCID: PMC8869288.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
41
#线粒体#
80
#肺动脉高压#
0
#线粒体功能#
53
#功能障碍#
32
#线粒体功能障碍#
42