Cell:重磅!一种肠道细菌有望逆转自闭症症状
2016-06-18 佚名 生物谷
在一项新的研究中,来自美国贝勒医学院的研究人员报道,缺乏一种特定的肠道细菌物种导致小鼠社交能力不足(social deficit)。这些社交能力不足令人想起人类自闭症谱系障碍(autism spectrum disorder, ASD)的症状。通过将这种细菌物种添加到受影响的小鼠肠道中,研究人员能够逆转这些小鼠的一些社交行为问题。相关研究结果发表在2016年6月16日那期Cell期刊上,论文

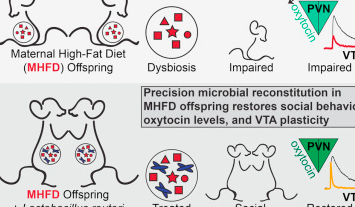
在一项新的研究中,来自美国贝勒医学院的研究人员报道,缺乏一种特定的肠道细菌物种导致小鼠社交能力不足(social deficit)。这些社交能力不足令人想起人类自闭症谱系障碍(autism spectrum disorder, ASD)的症状。通过将这种细菌物种添加到受影响的小鼠肠道中,研究人员能够逆转这些小鼠的一些社交行为问题。相关研究结果发表在2016年6月16日那期Cell期刊上,论文标题为“Microbial Reconstitution Reverses Maternal Diet-Induced Social and Synaptic Deficits in Offspring”。如今,研究人员正准备在未来的研究中探究益生菌对神经发育障碍的影响。
“其他研究小组正在试图使用药物或脑部电刺激来逆转与神经发育障碍相关联的一些行为症状,但是在这项新的研究中,我们可能有一种新方法”,论文通信作者、贝勒医学院神经科学副教授Mauro Costa-Mattioli博士说,“我们目前仍然不知道它是否能够在人体内有效,但是它一种非常令人激动的从肠道影响脑部的方法。”
这项研究的灵感来自人类流行病学研究,这些研究已发现怀孕期间孕妇肥胖可能增加小孩患上神经发育障碍(包括ASD)的风险。此外,一些ASD患者也表现出反复发作的胃肠道问题。随着不断有研究证实饮食如何能够改变肠道微生物组和肠道细菌如何影响脑部,Costa-Mattioli和他的同事们猜测这之间可能存在关联。
在开始这项研究时,研究人员给大约60只雌性小鼠喂食高脂肪膳食。他们培育这些小鼠,等待它们繁殖幼鼠。这些幼鼠与它们的母鼠在三周内呆在一起,然后转为吃正常的膳食。在一个月后,这些幼鼠表现出社交行为问题,比如花更少的时间与它们的同伴交往,不主动发起互动。
“首先,我们想要观察一下吃正常膳食的母鼠产下的幼鼠与吃高脂肪膳食的母鼠产下的幼鼠在肠道微生物组之间是否存在差异。因此,我们利用16S rRNA基因测序法确定它们肠道的细菌组成。我们发现它们之间存在显著的差别”,论文第一作者、Costa-Mattioli实验室博士后研究员Shelly Buffington说,“这些测序数据是如此具有一致性以至于通过研究单只小鼠的肠道微生物组,我们可能能够预测它的行为是否受到影响。”
Buffington接着测试微生物组中的这些细菌物种差异是否是吃高脂肪膳食的母鼠产下的幼鼠社交行为障碍的病因。鉴于小鼠有吃彼此粪便的习性,研究人员让这些小鼠住在一起,这样它们就能够获得它们同伴的肠道菌群。当吃高脂肪膳食的母鼠产下的社交行为受损的幼鼠与正常的小鼠为伴时,研究人员在4周内就观察到这些幼鼠的肠道微生物组完全恢复和同时发生的社交行为改善。研究人员作出结论:一种或多种有益细菌物种可能在正常的社交行为中发挥着重要作用。对无菌小鼠进行粪便移植实验提供因果关系的证据证实吃高脂肪膳食的母鼠产下的幼鼠肠道中不平衡的微生物生态环境是它们存在社交行为障碍的原因。
研究人员接下来想知道能够影响这些幼鼠的社交行为的特定细菌物种。全基因组鸟枪测序揭示出一种被称作罗伊氏乳杆菌(Lactobacillus reuteri)的细菌在吃高脂肪膳食的母鼠产生的幼鼠肠道微生物组中下降了9倍多。
Buffington说,“我们在体外培养最初从人奶水中分离出的一种罗伊氏乳杆菌菌株,将它添加到吃高脂肪膳食的母鼠产下的幼鼠喝的水中。我们发现添加这单种细菌菌株能够逆转这些幼鼠的社交行为。”其他的ASD相关性行为,如焦虑,并没有因为这种细菌重建而得到逆转。有趣的是,研究人员发现罗伊氏乳杆菌也促进“融合激素(bonding hormone)” 催产素(oxytocin)产生,其中已知催产素在社交行为中发挥着关键性作用,而且与人类自闭症相关联。
研究人员想知道社交行为受损的幼鼠的奖赏回路(reward circuitry)是否存在功能障碍。“我们发现作为对社会互动的反应,相对于正常的对照幼鼠,这些幼鼠脑部中的一个关键性奖赏区域缺乏突触强化(synaptic potentiation),” Costa-Mattioli说,“当我们将这种细菌放回到吃高脂肪膳食的母鼠产下的幼鼠体内,我们也能够恢复这种奖赏回路中发生的突触功能变化。”
研究人员认为他们的研究发现---利用一种人类细菌物种促进催产素释放和改善社交行为受损的小鼠的社交行为障碍---可能为开发一种益生菌介入方法治疗人类神经发育障碍奠定基础。
原始出处
Shelly A. Buffington, Gonzalo Viana Di Prisco, Thomas A. Auchtung, Nadim J. Ajami, Joseph F. Petrosino, Mauro Costa-Mattioli.Microbial Reconstitution Reverses Maternal Diet-Induced Social and Synaptic Deficits in Offspring.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
30
#CEL#
34
不错,能找到相关的信息
0
#肠道细菌#
22
#自闭#
28
#重磅#
23
赞?
86
赞?
59
发现不错
99
值得研究
133