JCEM:胰岛素抵抗与甲状腺结节血管化存在关联
2014-11-05 MedSci MedSci原创
研究背景: 胰岛素抵抗是甲状腺结节生长和进展的重要影响因素,可能与结节血管化的分布、组成及密度有关。 研究目的: 研究胰岛素抵抗与甲状腺结节血管化之间的关系。 研究设计: 2011年6月至11月,在中国南京开展了一项基于人群的横断面研究。 受试者: 研究共对40-79岁的10050名参与者进行检查,共检出2886例甲状腺结节患者,另纳入2532例符合纳入标
研究背景:
胰岛素抵抗是甲状腺结节生长和进展的重要影响因素,可能与结节血管化的分布、组成及密度有关。
研究目的:
研究胰岛素抵抗与甲状腺结节血管化之间的关系。
研究设计:
2011年6月至11月,在中国南京开展了一项基于人群的横断面研究。
受试者:
研究共对40-79岁的10050名参与者进行检查,共检出2886例甲状腺结节患者,另纳入2532例符合纳入标准的病例。
主要监测结局:
采用能量多普勒检测血流模式、阻抗指数(RI)和血管指数(VI)评价甲状腺结节的血管化情况(VI的计算说明见图1)。其他测量指标包括空腹胰岛素、空腹血糖、2小时口服糖耐量测试、HbA1c、HOMA-IR及体质指数等。
研究结果:
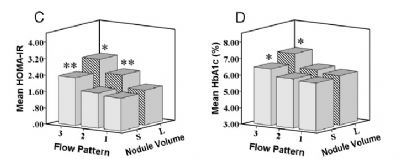
HOMA-IR和HbA1c与甲状腺结节的血流模式呈正相关(HOMA-IR: R=0.35, P<0.001; HbA1c: R=0.19, P<0.001)(见图2),并且这种正相关关系在大结节(体积≥0.2 ml)的患者中更为显著。此外,在大结节患者中,HOMA-IR和HbA1c还与RI(HOMA-IR: β=0.42, SE=0.03, R=0.43, P<0.001; HbA1c: β=0.22, SE=0.04, R=0.23, P<0.001)及VI(HOMA-IR: β=0.49, SE=0.05, R=0.53, P<0.001; HbA1c: β=0.34, SE=0.11, R =0.37, P<0.001)呈正相关关系。
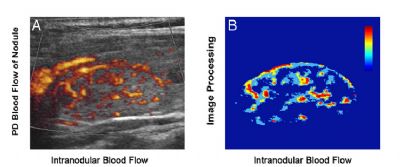
图1,A:一位42岁女性甲状腺结节B超横切面显示结节存在外周环状血流及内部血流。B:血管指数指图中彩色标记区域面积占整个结节面积的比例(外周血流不计算在内)。
图2,(C,D)平均HOMA-IR、HbA1c水平与不同体积大小甲状腺结节血流模式的关系
研究结论:
胰岛素抵抗及高血糖与甲状腺结节的血流模式、阻抗指数和血管指数呈正相关关系,在大结节患者中这种相关性更为显著。研究提示胰岛素抵抗在甲状腺结节血管化的分布、组成及密度中起关键作用,并可能促进甲状腺结节的生长和进展。
原始出处:
Kun Wang, Yu Yang, Yang Wu, Jie Chen, Danyu Zhang, Xiaodong Mao,Xinping Wu, Xianqin Long, and Chao Liu. The association between insulin resistance and vascularization of thyroid nodules. JCEM, Nov 04, 2014.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好好学习学习
124
#JCEM#
31
#胰岛#
39
#JCE#
35
#血管化#
29