MAYO Clin Proc:他汀类药物可以减少严重的细菌性血液感染风险
2017-10-03 佚名 medicalxpress
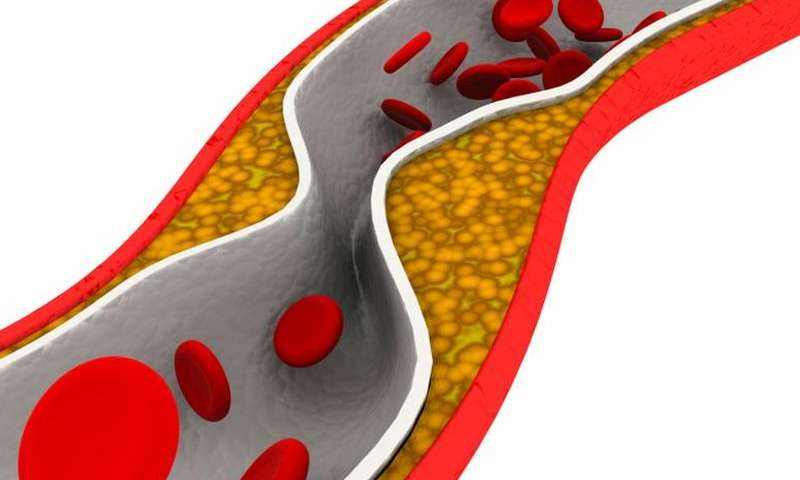
他汀类药物不仅可以预防心脏疾病的风险,还能将感染金黄色葡萄球菌的风险减少27%。研究人员报告说,他汀类药物的使用,尤其是先前存在慢性病,如糖尿病,肾脏病,肝脏疾病的老人患者中,可以预防严重的血液感染。随着世界人口的老龄化,越来越多的人患有慢性病,任何潜在的预防都可能具有重要的临床意义。
- Circulation:依泽替米贝联合他汀药物能明显降低ACS患者卒中风险
- NEJM:阿托伐他汀治疗动脉粥样硬化并不会增加冠脉疾病的发生风险
- Atherosclerosis:性别和年龄影响他汀的降脂效果?
- J Am Geriatr Soc:他汀类药物跻身“万能药”行列,显著降低老年人死亡率
- 美国医生关于脑卒中后使用他汀的思考:可能不是每个人都需要
- JAHA:高强度他汀治疗外周动脉疾病疗效更好?
- Chest:阿托伐他汀能减轻铜绿假单胞菌感染支气管扩张患者的炎症
- Gastroenterology:结肠癌确诊患者服用他汀能降低死亡风险
- Scand J Urol:他汀类药物使用与雄激素剥夺疗法治疗前列腺癌恶化的关系
- 【ESC 2017】EMPATHY研究质疑糖尿病视网膜病变患者强化他汀治疗的效果
- 【ESC 2017】REVEAL研究表明他汀联合anacetrapib可降低高危患者心血管事件的发生
- Int J Cancer:糖尿病、使用他汀类药物和二甲双胍对癌症患者的死亡率的影响有哪些?
- JACC:如何减少他汀类使用中出现的肌肉毒性等副作用?
- 【ESC 2017】女性较少接受指南推荐的他汀类药物剂量来预防心血管事件
- ESC大会:接受他汀类药物治疗的女性更不容易得乳腺癌? 更多信息请点击:有关他汀更多资讯
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ROC#
29
#血液感染#
51
#他汀类药#
28
学习学习.继续关注
53
学习学习.了解了解
48
#PRO#
23
学习
57
henhao
44
老药新用途.可以好好研究
55
学习.谢谢分享
24