Br J Cancer:RON促进ESR1突变型乳腺癌的治疗耐药性
2020-12-09 xiaozeng MedSci原创
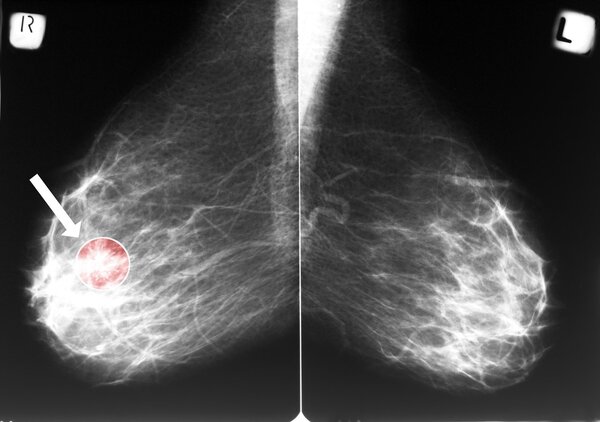
全球每年有超过60万妇女死于转移性乳腺癌(MBC)。尽管有效的内分泌治疗和靶向疗法可以用于雌激素受体(ER)阳性乳腺癌(BC)的治疗,但仍有20%的妇女出现癌症的复发和/或转移。
全球每年有超过60万妇女死于转移性乳腺癌(MBC)。尽管有效的内分泌治疗和靶向疗法可以用于雌激素受体(ER)阳性乳腺癌(BC)的治疗,但仍有20%的妇女出现癌症的复发和/或转移。
ER阳性MBC患者在转移环境中接受AI(芳香化酶抑制剂)治疗后,经常会出现ESR1(雌激素受体1)突变。该基因突变也是内分泌治疗(ET)耐药的最常见机制,其特征是具有激素超敏或配体依赖性的转录活性。
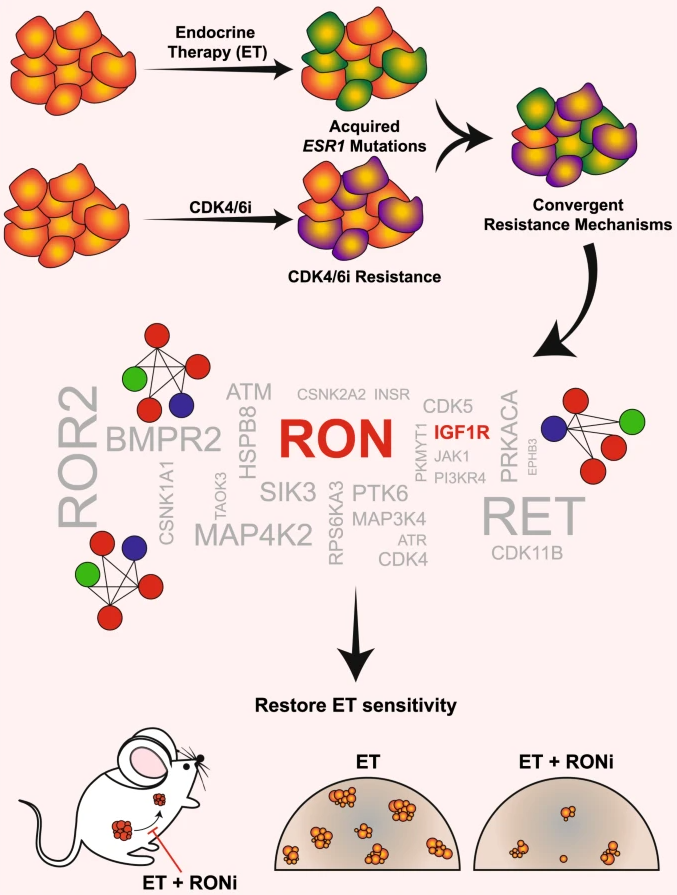
研究示意图
获得性ESR1突变对应着患者的不良预后,且缺乏有效的针对这些癌症的选择性治疗策略。因此,在ESR1突变型癌症中鉴定潜在的治疗靶标对于更好地控制转移性疾病是必需的。
研究人员通过在ESR1 Y537S突变型细胞中进行蛋白质组学分析,以鉴定ESR1突变细胞中的超活化激酶。通过磷酸化免疫印迹实验、类器官生长实验以及人源移植瘤(PDX)转移模型发现,RON和PI3K高度活跃。
ESR1突变模型显示雌激素非依赖性的生长和转移倾向
研究人员发现,RON在ESR1突变模型以及获得性PalbR(Palbociclib耐药)模型中被过度激活。药理学和遗传学抑制结果显示,RON能够与IGF-1R(胰岛素样生长因子1受体)相互作用,并受突变型ER调节,该结果由内分泌治疗(ET)磷酸化蛋白表达水平降低所证实。
RON抑制剂(RONi)与ET的联合治疗能够减少ESR1突变型类器官的生长,并在PalbR模型中作为单一疗法表现出治疗的功效。ET与RONi的联合治疗能够显著减少ESR1 Y537S突变型PDX模型的转移。
抑制RON信号通路能够恢复ET的敏感性
综上,该研究结果表明,抑制RON/PI3K通路或可成为ESR1突变型和PalbR MBC患者的潜在的有效治疗策略。而临床上的数据预测显示,ET的耐药机制也可能导致CDK4/6抑制剂的耐药。
原始出处:
Dustin, D., Gu, G., Beyer, A.R. et al. RON signalling promotes therapeutic resistance in ESR1 mutant breast cancer. Br J Cancer (01 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#突变型#
36
#ESR1#
39
非常好
60
学习学习!
79
学习
82
受益匪浅
87
有意义
97
身边很多女性受到乳腺结节,肿瘤的疾病困扰,希望可以有治疗的最好的治疗方案,让患者受益。
77
学习学习
38
学习
45