J Immunol:TNF反向信号调节炎症反应分子机制
2016-01-11 佚名 生物谷
TNF-a是一类典型的炎性细胞因子,它的前体是一类II型跨膜蛋白(mTNF-a)。成熟的TNF-a能够识别细胞表面的TNF-R1以及TNF-R2,从而使得该类受体的激活与三聚化。类似的,TNF-a前体有两类截然不同的功能:由于mTNF-a在未结合受体的情况下是天然的三聚化结构,一方面它可以像成熟的TNF-a一样与TNF-R结合产生下游信号,另一方面这一结合也可以使其将受体信号反向传递至配体细胞中(
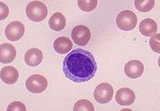
TNF-a是一类典型的炎性细胞因子,它的前体是一类II型跨膜蛋白(mTNF-a)。成熟的TNF-a能够识别细胞表面的TNF-R1以及TNF-R2,从而使得该类受体的激活与三聚化。类似的,TNF-a前体有两类截然不同的功能:由于mTNF-a在未结合受体的情况下是天然的三聚化结构,一方面它可以像成熟的TNF-a一样与TNF-R结合产生下游信号,另一方面这一结合也可以使其将受体信号反向传递至配体细胞中(即相反方向)。之前的研究已经发现mTNF-a的反向信号能够干预LPS对巨噬细胞的激活作用,其中的关键步骤包括ERK的激活。然而,其中的分子机制并不清楚。在最近的一项研究中,来自希腊Debrecen大学的Zsuzsa Szondy课题组阐释了TNF-a反向信号的最新分子机制。相关结果发表在最新一期的Journal of Immunology杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#炎症反应#
22
#TNF#
32
赞
58
信号
118
赞
100