我国学者在《Annals of Oncology》发表高分SCI文章,展示非小细胞肺癌的精准治疗方案
2017-07-07 MedSci MedSci
近日,国际经典肿瘤学临床期刊《肿瘤学年鉴》(Annals of Oncology,SCI影响因子11.855)以短文(Letter)的形式发表来自我国学者在非小细胞肺癌治疗方面的最新研究成果,这也是中国肺癌临床经验在国际肿瘤靶向治疗领域的又一次高质量展示。文章概述一名36岁无烟史中国女性于2016年6月确诊为肺腺癌IV期,并伴多发转移,化疗无效,ctDNA检测显示患者携带EGFR L858R和
近日,国际经典肿瘤学临床期刊《肿瘤学年鉴》(Annals of Oncology,SCI影响因子11.855)以短文(Letter)的形式发表来自我国学者在非小细胞肺癌治疗方面的最新研究成果,这也是中国肺癌临床经验在国际肿瘤靶向治疗领域的又一次高质量展示。
文章概述
一名36岁无烟史中国女性于2016年6月确诊为肺腺癌IV期,并伴多发转移,化疗无效,ctDNA检测显示患者携带EGFR L858R和扩增变异,于7月初开始转用厄洛替尼后,临床症状显着缓解,脑转移灶消失(CR),肺和肝部病灶缩小(PR)。半年后疾病进展;第二次ctDNA检测结果显示,患者新增c-MET扩增,随后开始厄洛替尼与克唑替尼联合用药,临床症状缓解,且肺部病灶显着缩小。联合用药9周后,患者再次出现疾病进展;第三次ctDNA检测结果显示,患者新发NRAS Q61H和KRAS G12D变异;MET扩增未检到,但检出了一个尚未报道的MET G1108C错义突变;G1108残基位于MET克唑替尼结合区域,突变后可能影响药物结合导致克唑替尼耐药。
文章亮点
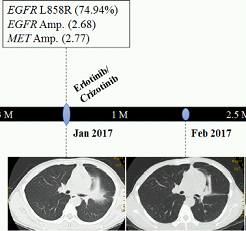
亮点一:厄洛替尼/克唑替尼联用效果显着,具有临床可行性
患者ctDNA二代测序检出EGFR L858R突变和基因扩增、以及继发性c-MET扩增后,开始厄洛替尼/克唑替尼联合用药,之后患者咳嗽减轻,临床症状缓解,血清癌标下降,且肺部病灶显着缩小。
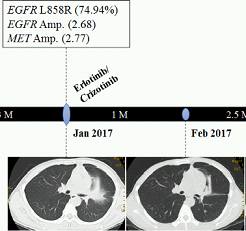
图1. 肺部原发灶联合用药前后CT影像图
亮点二:新的克唑替尼潜在耐药位点——METG1108C突变
厄洛替尼/克唑替尼联合用药耐药后,ctDNA二代测序检出了一个尚未报道过的METG1108C错义突变。蛋白三维结构模拟分析发现,G1108残基位于c-MET与克唑替尼的结合位点附近,突变后可能影响药物结合,从而导致克唑替尼耐药。
图2. MET-克唑替尼结合三维模拟图
亮点三:厄洛替尼对脑部病灶效果显着
ctDNA二代测序检出EGFR L858R和基因扩增,患者服用厄洛替尼后,临床症状迅速缓解,尤其是脑转移灶病灶消失(CR,图3)。这说明厄洛替尼入脑效果良好,对EGFR突变阳性的肺癌脑转移灶效果显着。但是纵观患者整个病程,疾病进展时EGFR变异丰度一直处于较高水平,厄洛替尼对其他EGFR变异阳性病灶治疗效果仍需进一步研究和讨论。

图3. 克唑替尼用药前后脑转移灶MRI影像图
亮点四:通过二代基因测序检测ctDNA中基因拷贝数变化(CNV)具有可行性
本案例中多次ctDNA二代测序均可检出CNV,对应调整的用药方案也获得了预期的临床响应。这说明渥恩ctDNA二代测序检测技术可实现CNV精准分析,对患者临床用药具有宝贵的参考价值。
亮点五:ctDNA二代测序可实时地、全面准确地反应患者的突变情况
ctDNA具有无创易获取等优点,其在机体耐药、疾病进展等关键节点发挥了关键作用,能辅助临床及时调整用药方案并进行肿瘤监控;二代测序具有通量高、检测灵敏、无需预先知道核酸序列等优点,可以辅助临床发现新肿瘤耐药机制,实现临床科研双向转化。
ctDNA检测
ctDNA检测在患者的临床诊断和耐药性检测上发挥着不可替代的作用。但是,目前ctDNA量少、半衰期短、片段较短,其含量受肿瘤种类、位置、分期等影响,检测难度极大。通过优化的超微量捕获技术进行DNA抽提及建库,使用自主研发的分子标签技术进行纠错和去重,使检测结果准确率提高10倍以上,在得到测序数据后采用背景降噪技术优化分析算法,将待测样本数据中的周期性错误作为背景进行消除,可大幅提高低频突变的检出率。通过以上技术优势及优化处理,并采用更严谨的质控标准来提高数据的质量和结果的准确性。在ctDNA二代测序针对不同突变类型的检测效果如下:

本研究成果是由渥恩医学联合广州医科大学第二附属医院李宇清组联合完成。渥恩医学医学部的宋姗姗和张晓宇参与了本项目的具体工作,其中宋姗姗为本文的共同第一作者。
渥恩医学和李宇清教授长期致力于TKIs临床治疗和耐药机制的研究,此例临床实践的发表对用ctDNA二代测序进行肿瘤监控并指导个性化用药具有临床指导意义
这次高质量研究成果发表标志着渥恩医学的循环肿瘤DNA(ctDNA)二代基因测序技术(NGS)亦获得了国际同行的认可。
关于《Annals of Oncology》期刊:
Annals of Oncology由欧洲医学肿瘤协会和日本医学肿瘤协会主办,是由牛津大学出版的同行评审性质的临床医学期刊,主要发表对临床肿瘤学和肿瘤基础研究具有重大意义的医学研究新成果、综述文章等。2016年最新数据显示该期刊IF已达11.855,在300多肿瘤领域期刊跻身前十,为顶级SCI期刊之一。
关于渥恩医学:
上海渥恩生物科技有限公司是一家专注于研发肿瘤诊断和精准治疗的科技型公司,基于临床和基因组大数据,为医疗机构和肿瘤患者带来优化和精确的医疗解决方案。
渥恩生物拥有全球领先的临床二代基因检测技术及液体活检技术,其独家的AccuTarget分子标签技术、微量建库捕获技术及生物医学大数据(AMGO Touch)平台,可为医疗机构及科研单位提供实时的、在线的临床诊断及科研服务。
渥恩本着“精准先行,患者至上”的宗旨,使每位患者尽早诊断,获得合适的治疗方案,延长生命、提高生活质量是渥恩不断努力的方向。
请点击此处下载原文 mdx324-clean PDF.pdf
mdx324-clean PDF.pdf
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#治疗方案#
28
#Oncology#
33
#非小细胞#
28
#Oncol#
30
#我国学者#
39
谢谢分享,学习了
73
不错的文章不错的文章
78
大师写的太微妙了,让国人振奋
77
能用靶向药,连续多次测序,精准医学呀
77
学习了
75