JAHA::一个全新的自发性肺动脉高压小鼠模型
2021-11-03 刘少飞 MedSci原创
SIRT3(脱乙酰酶)和 UCP2(非典型解偶联蛋白)的孤立功能丧失单核苷酸多态性 (SNP) 与肺动脉高压 (PAH) 和胰岛素抵抗有关,研究提供了一种新的 PAH 小鼠模型及其PAH 小鼠特征。

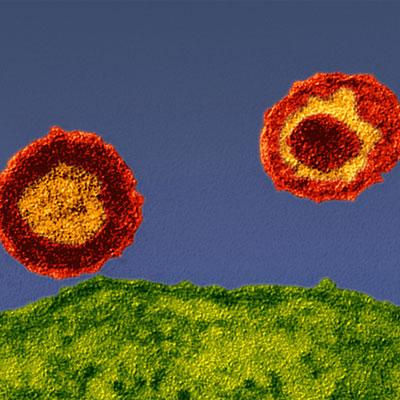
肺动脉高压 (PAH) 的特征是肺动脉重塑,导致管腔闭塞,增加肺血管阻力 (PVR)。 虽然最初这会导致右心室 (RV) 肥大,但随后会导致 RV 扩张并因 RV 衰竭而死亡。关于PAH的代谢理论表明,线粒体抑制是一个关键的早期事件,它也有可能激活许多与 PAH 相关的转录因子。线粒体氧化磷酸化(葡萄糖氧化)的抑制是 T 细胞活化的早期和必要事件。事实上,在 PAH 患者的骨骼肌活检中,有证据表明存在线粒体功能障碍(线粒体酶下调和糖酵解酶上调)。研究发现,缺乏 Sirt3 (sirtuin3)11(一种主要的线粒体脱乙酰酶)或 Ucp2(解偶联蛋白 2)(一种主要促进钙进入线粒体的非典型解偶联蛋白)的 KO 小鼠发生了自发性肺动脉高压(PHT)和血管重塑。
本研究目的:针对SIRT3和 UCP2的孤立功能丧失单核苷酸多态性及胰岛素抵抗的动物模型及患者的探索。
研究方法:
在 PAH 患者(n=60)的前瞻性队列中,该研究测量了 SIRT3 和 UCP2 的 SNP,以及几个临床特征,包括侵入性血流动力学数据。
研究结果:该研究发现 SIRT3 和 UCP2 SNP 通常以纯合子或杂合子的方式出现在同一患者中,与 PAH 的严重程度呈正相关,并与 2 型糖尿病的存在和10 年结果(死亡和移植)相关。
PAH 患者中的 SIRT3 和 UCP2 单核苷酸多态性 (SNP)

Sirt3 和 Ucp2 缺失对小鼠杂合子或纯合子 PAH 严重程度的基因剂量依赖性影响

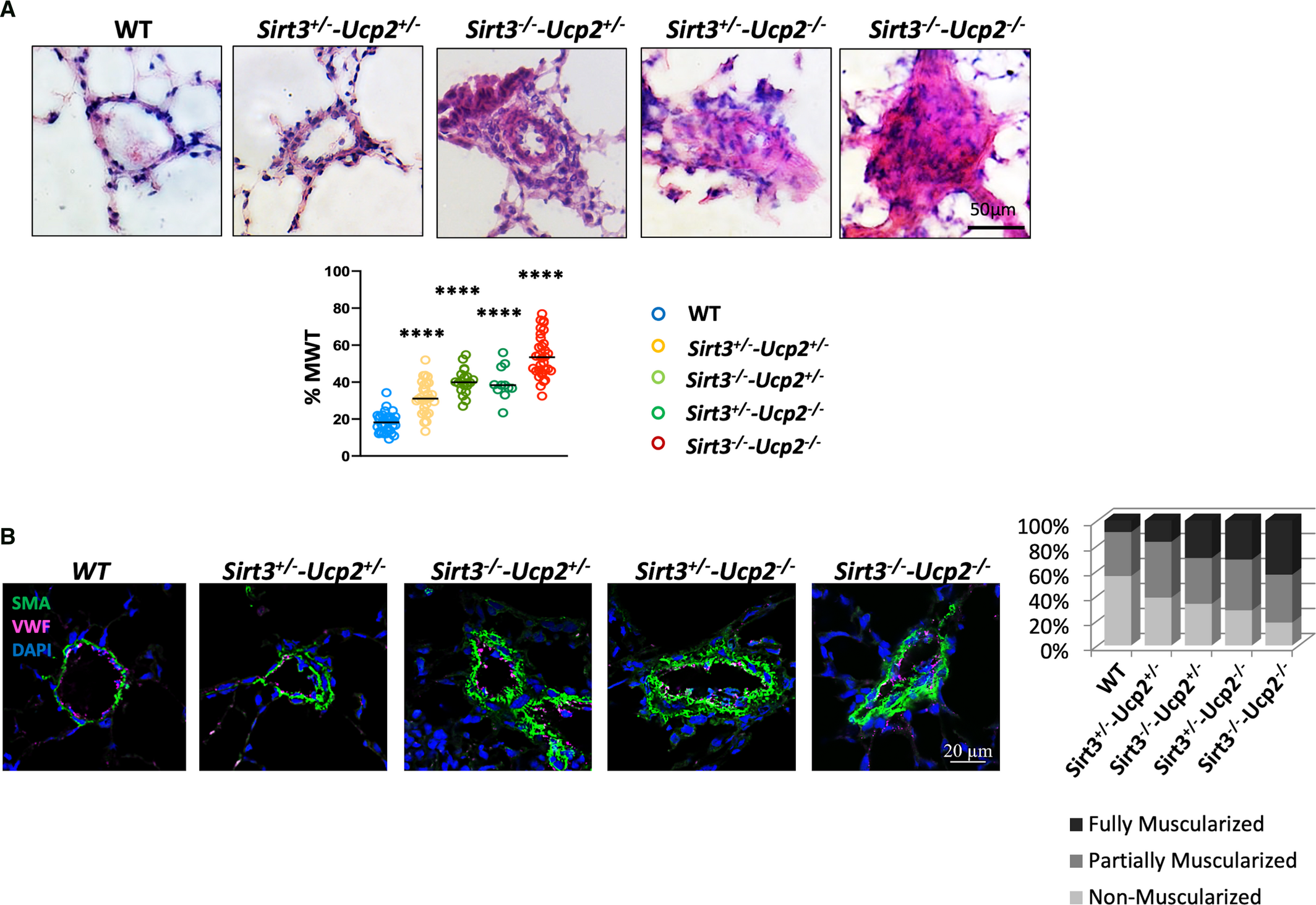
Sirt3 和 Ucp2 缺失的杂合子或纯合子小鼠的肺血管重塑
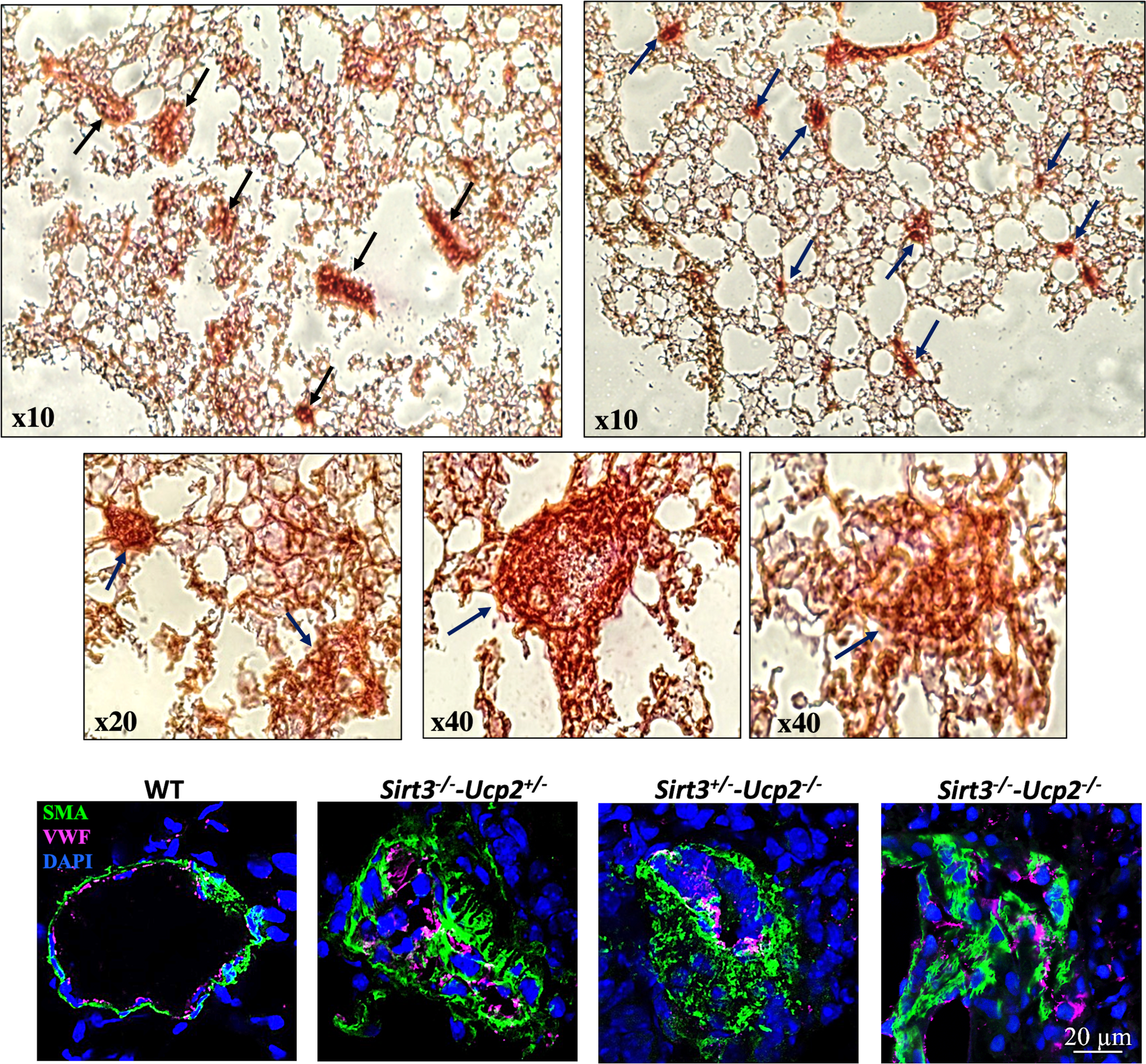
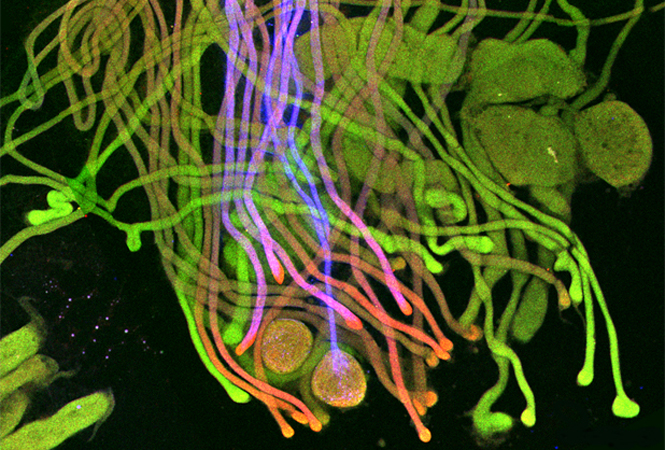
缺乏 Sirt3 和 Ucp2 的小鼠的丛样动脉病变
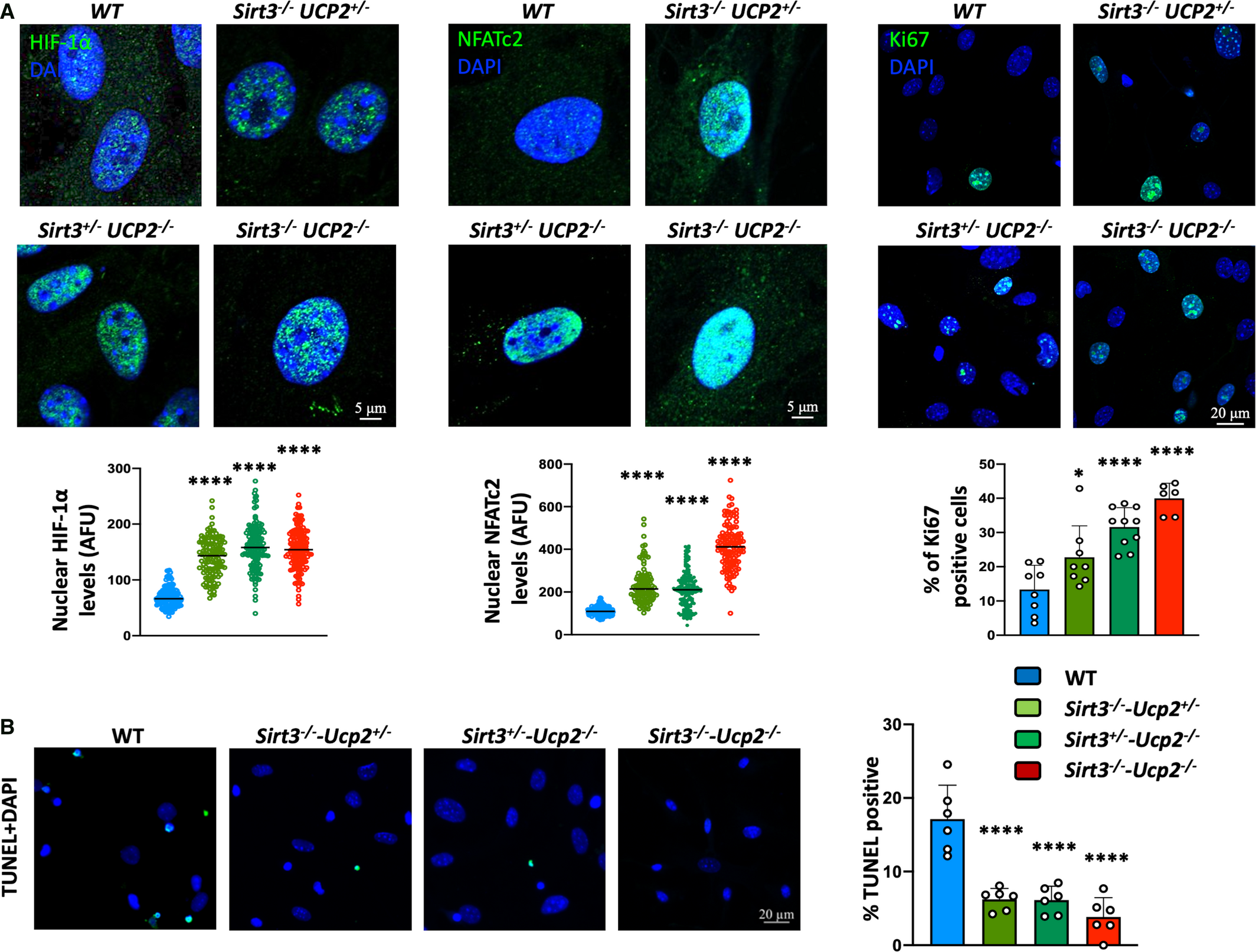
来自Sirt3 和 Ucp2 的缺失小鼠杂合子或纯合子的培养的 PASMC 的增殖和抗凋亡表型
缺乏 Sirt3 和 Ucp2 的小鼠 PASMC 的代谢重塑

为了从机制上探索这一点,以上是针对 Sirt3 和 Ucp2 生成了双敲除小鼠,并发现 PAH 的严重程度增加(平均肺动脉压力、右心室肥大/扩张和广泛的血管重塑,包括炎症性丛样病变,以基因剂量依赖性方式),以及胰岛素抵抗,与野生型小鼠相比。与野生型小鼠相比,双敲除肺动脉平滑肌细胞的线粒体功能受到抑制(呼吸减少、线粒体膜电位增加)与细胞凋亡抵抗和增殖增加有关。
研究结论:
该研究发现支持PAH 的代谢理论,并表明这些小鼠表现出模仿人类 PAH 的自发性严重 PAH(没有环境或化学触发因素),并且可以解释我们患者队列中的发现。研究提供了一种新的 PAH 小鼠模型,具有其他 PAH 小鼠模型中通常不存在的人类疾病的几个特征。该小鼠模型支持我们队列中具有挑战性的临床数据,并且与在编码线粒体蛋白的基因中携带超过 1 个功能丧失 SNP 的 PAH 患者亚组直接相关,特别是那些在两个等位基因中都携带它们的基因。
文献出处:
Zhang Y, Zervopoulos SD, Boukouris AE, Lorenzana-Carrillo MA, Saleme B, Webster L, Liu Y, Haromy A, Tabatabaei Dakhili SA, Ussher JR, Sutendra G, Michelakis ED. SNPs for Genes Encoding the Mitochondrial Proteins Sirtuin3 and Uncoupling Protein 2 Are Associated With Disease Severity, Type 2 Diabetes, and Outcomes in Patients With Pulmonary Arterial Hypertension and This Is Recapitulated in a New Mouse Model Lacking Both Genes. J Am Heart Assoc. 2021 Oct 30:e020451. doi: 10.1161/JAHA.120.020451. Epub ahead of print. PMID: 34719264.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉高压#
41
#AHA#
41
#小鼠模型#
50
#自发性#
48