BMC Cardiovasc Disord:中国瓣膜病的现状和病因:阜外医院一项基于大样本人群的调查
2021-07-16 “心关注”公众号 “心关注”公众号
过去50年,世界范围内的瓣膜性心脏病(VHD)流行率变化较大。在发展中国家,风湿性心脏病仍是主要问题,而发达国家则面临更多退化性病变导致的瓣膜性心脏病。
过去50年,世界范围内的瓣膜性心脏病(VHD)流行率变化较大。在发展中国家,风湿性心脏病仍是主要问题,而发达国家则面临更多退化性病变导致的瓣膜性心脏病。
中国曾一度被认为风湿性心脏病的发病率较高,但自1978年改革开放以来,随着物质生活条件的改善,这一状况已有所缓解。然而,随之将至的老龄化社会,又将退行性瓣膜性心脏病的防控治提上日程。
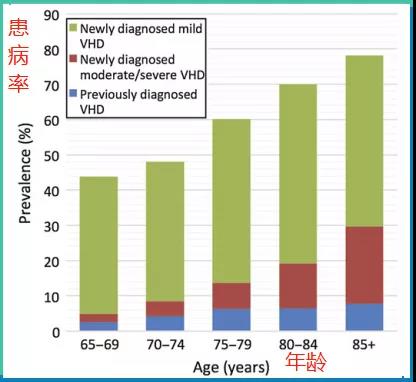
图片:各年龄层人群的瓣膜性心脏病患病率
2006年,一项基于人群的研究有报道,美国成人的瓣膜性心脏病患病率为2.5%。2016年,英国一项专业调查统计得出,65岁以上老年人群的瓣膜性心脏病患病率已高达51%,其中包括了6.4%未被诊断的中重度瓣膜性心脏病患者。
目前,国内对瓣膜性心脏病的病因及严重程度报道有限,仅单一省份或地区有过报道。近日,中国医学科学院阜外医院高润霖院士、王增武教授共同通讯发表在《BMC Cardiovasc Disord》杂志上的文章,通过全国性大样本人群的超声心动图数据,评估分析了我国瓣膜性心脏病的现状和病因。
该项全国性调查选取了国内35岁以上的34994例参与者,平均年龄51.8岁,女性占比49.3%。
其中,瓣膜性心脏病患者的平均年龄相对较高,心脏病史更为普遍,除糖尿病外的其他多项疾病(高血压、卒中、血脂异常、慢性肾病)合并率较高。
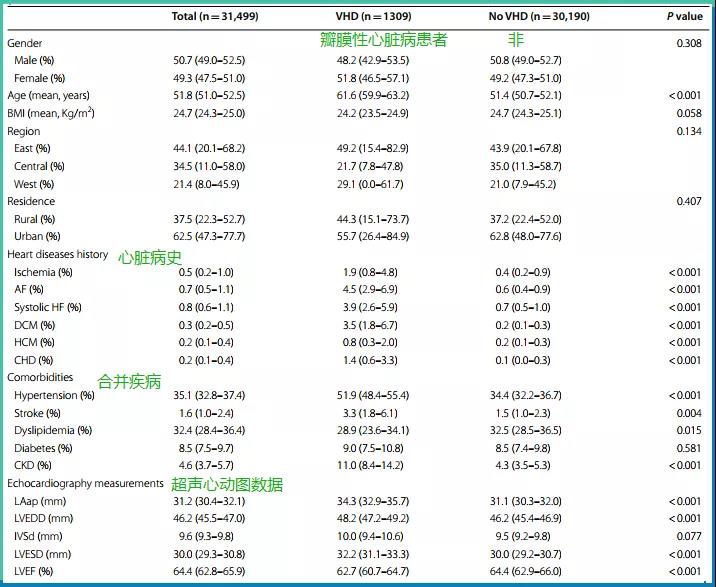
图1:有/无瓣膜性心脏病人群的基线数据
根据2010年全国普查数据,国内约有25621503例瓣膜性心脏病患者,加权患病率为3.8%。瓣膜性心脏病的患病率随年龄的增长而有所增加,男女之间无显着差异。
其中,高血压与非高血压人群的瓣膜性心脏病患病率对比为5.6% vs 2.8%,差异显着;慢性肾病与非慢性肾病人群的瓣膜性心脏病患病率对比为9.2% vs 3.5%,差异同样显着。
总的来说,比较常见的瓣膜性心脏病患病率统计如下:
主动脉反流(AR,1.2%),二尖瓣反流(MR, 1.1%),三尖瓣反流(TR, 0.8%), 二尖瓣狭窄(MS, 0.8%)。
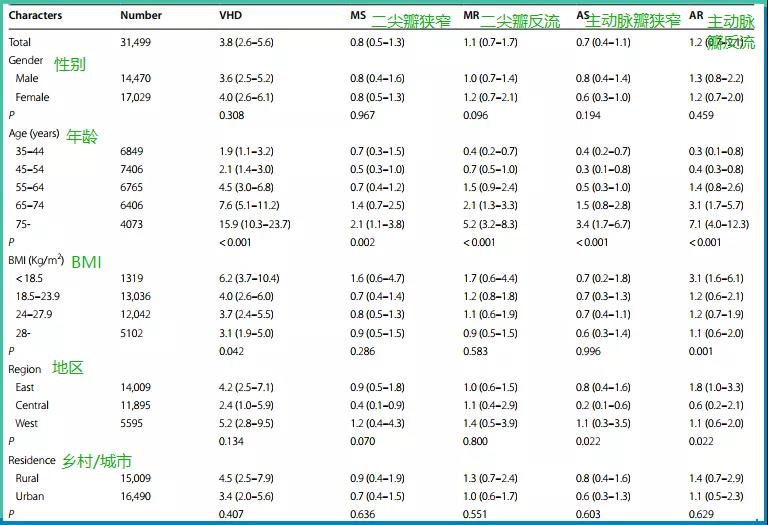
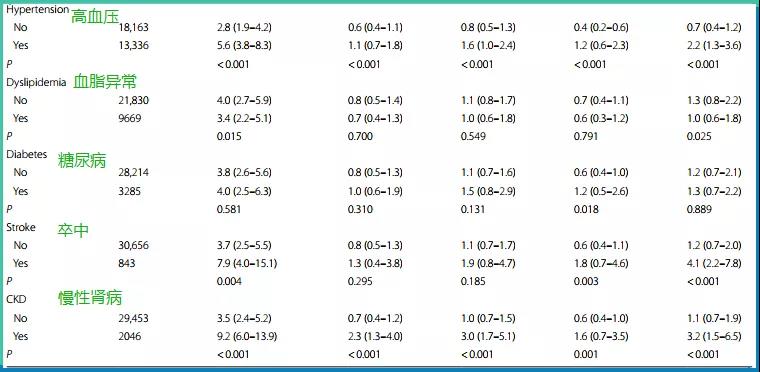
图2:各特征人群左心瓣膜性心脏病的发病率统计及风险对比
研究者对不同年龄层患者的瓣膜性心脏病病因构成做了统计:
从总体患者来看,风湿性心脏病排在首位,构占比高达55.1%。在35-44岁患者中,构占比高达77.8%,而到了75岁以上患者,滑至38%。
退行性瓣膜性心脏病在瓣膜性心脏病中的总构占比为21.3%。55-64岁患者中为18.2%,75岁以上患者中上升到了42.5%。
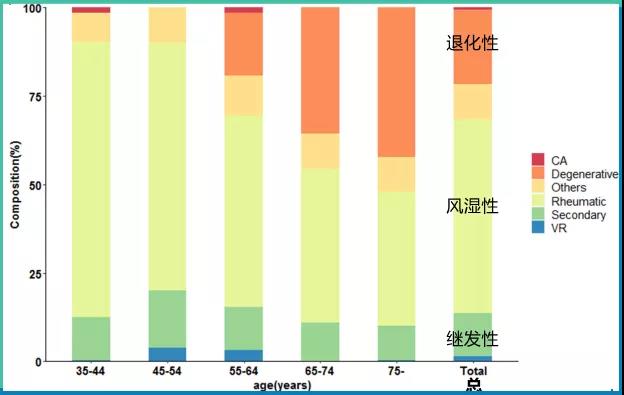
图3:不同年龄层瓣膜性心脏病患者的各病因构占比
另外,继发性瓣膜性心脏病,在瓣膜性心脏病中的总构占比为12.1%。
进一步看各年龄层中,退行性瓣膜性心脏病与风湿性心脏病在不同性别患者中的患病率:
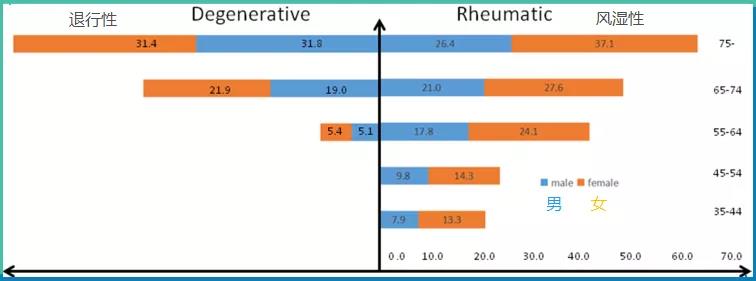
图4:瓣膜性心脏病的两种常见病因,在不同性别和年龄患者中的患病率
可明显看出,退行性与风湿性心脏病均呈现典型的倒金字塔形。
通过多元logistic回归分析发现,瓣膜性心脏病与年龄、高血压呈正相关,与BMI则呈负相关。
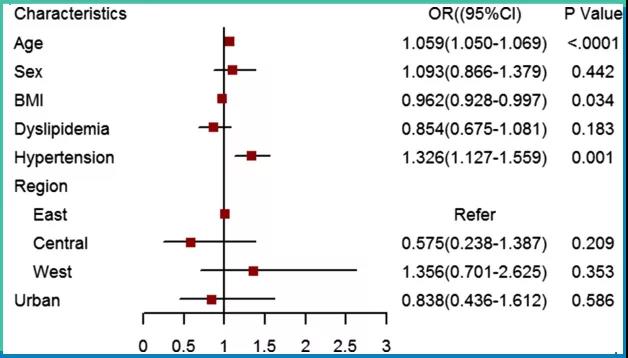
图5:用logistic回归计算瓣膜性心脏病的相关因素
此外,单一瓣膜功能障碍中,以主动脉瓣功能障碍(包括狭窄或反流)最为常见,其次是二尖瓣功能障碍。
最常见的双瓣膜功能障碍为主动脉瓣病变合并二尖瓣病变,三瓣膜功能障碍为主动脉瓣病变、二尖瓣病变合并三尖瓣病变。
在我国,尽管近些年来风湿性心脏病的患病率已有所下降,但仍是瓣膜性心脏病的首要病因,而退行性瓣膜性心脏病的患病率则出现了显着上升。
其中,主动脉瓣反流、二尖瓣反流是最常见的瓣膜功能障碍。
年龄和高血压是筛查及预防瓣膜性心脏病的重要标志因素。
原始出处:
Ying Yang, et al. Current status and etiology of valvular heart disease in China: a population-based survey. BMC Cardiovasc Disord. (2021) 21:339.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#阜外医#
38
#ASC#
27
#BMC#
31
#样本#
44
#Disord#
37
#Dis#
28
#阜外医院#
64
#瓣膜#
32