Breast Cancer Res Treat:新的猜想:雌孕激素比例失调可能与乳腺癌的发生有关
2014-11-25 medsci MedSci原创
Breast Cancer Res Treat:新的猜想:雌孕激素比例失调可能与乳腺癌的发生有关 肥胖与多种恶性肿瘤发生有关,然而多年来困扰我们的一个难题是:为什么肥胖增加绝经后女性乳腺癌的发生,却减少绝经前乳腺癌的发生?伦敦大学的Mitch Dowsett和Elizabeth Folkerd将给大家揭开这个谜底。 1.
肥胖与多种恶性肿瘤发生有关,然而多年来困扰我们的一个难题是:为什么肥胖增加绝经后女性乳腺癌的发生,却减少绝经前乳腺癌的发生?伦敦大学的Mitch Dowsett和Elizabeth Folkerd将给大家揭开这个谜底。
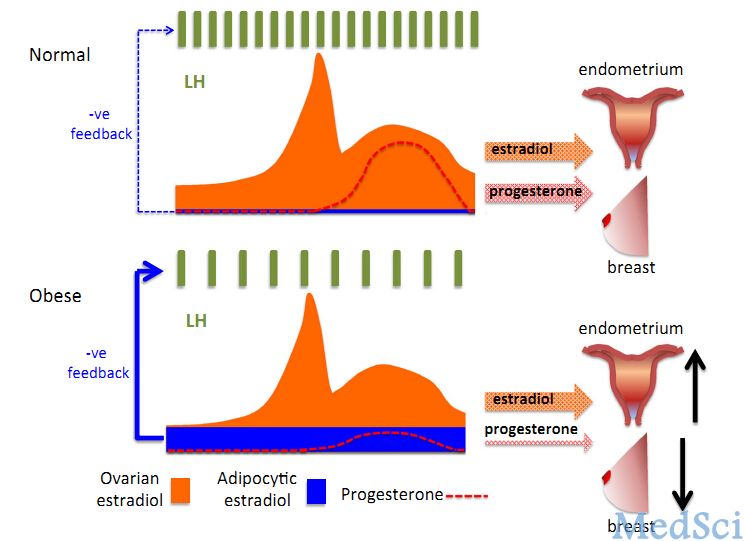
1.雌激素来源:女性卵巢和皮下脂肪在芳香化酶作用下产生雌激素,绝经前女性卵巢性激素的产生和卵泡的发育通过反馈系统(卵泡刺激素FSH、促黄体生成素LH)呈周期性变化,绝经后卵巢功能停止,因此雌激素来源于皮下脂肪。
2.绝经前肥胖女性孕激素水平与乳腺癌低风险有关:这个猜想来源于7年前的一个研究:该研究纳入24名月经正常的女性(12名正常BMI vs 12名高BMI),在一个月经周期的每日清晨采集中段尿测定其雌激素和孕激素代谢物(葡萄糖苷酶雌酮E-G和孕二醇葡萄糖苷酸P-G),结果两组E-G水平并没有差别,而P-G水平在高BMI组显著低于BMI正常组(P=0.002),当行减肥手术后,黄体P-G的水平上升。
肥胖女性产生过多的雌激素通过负反馈系统使促性腺激素减少,因此卵巢功能受抑制,从而使孕激素合成减少,而孕激素可促进成年女性乳腺发育。根据妇女健康倡议(WHI)和百万妇女(Million Women)的研究:绝经后女性服用雌激素和孕酮比只用雌激素女性有更高的患乳腺癌风险和更高乳腺密度,因此有理由认为绝经前肥胖女性较低的孕激素水平与乳腺癌低风险有关。
然而对于高BMI女性,绝经前和绝经后患子宫内膜癌风险同样高。对于高BMI绝经后女性,高雌激素水平的刺激被认为增加子宫内膜癌风险;对于绝经前女性,孕激素对于子宫内膜癌的发生是一个保护因素,高BMI绝经前女性的低孕激素水平增加患子宫内膜癌风险。
3.可能的机制:绝经前肥胖女性促黄体生成素减少,因此性腺产生的孕激素减少,这是绝经前肥胖女性患乳腺癌的保护因素和患子宫内膜癌的危险因素。本猜想真实性有待进一步研究,如果属实,可能对预防绝经前女性乳腺癌有帮助。
原始出处:
Dowsett, M. and E. Folkerd, Reduced progesterone levels explain the reduced risk of breast cancer in obese premenopausal women: a new hypothesis. Breast Cancer Res Treat, 2014.
本文是MedSci原创编译整理,欢迎转载! 转载请注明来源并附原文链接。谢谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








好好学习学习
135
#AST#
44
#TREAT#
46
#Breast#
42
#孕激素#
28