Sci. Transl. Med.:感染前免疫系统的组成影响SIV感染后疾病进展
2012-06-17 bo 生物谷
5月30日,Sci. Transl. Med.杂志报道,科学家发现感染前免疫系统的组成对猿猴免疫缺陷病毒(SIV)感染后疾病的进展具有显著影响。这为HIV的研究提供了新的线索。 某些HIV患者对该病毒的抵抗性很强,而有些患者则进展迅速。其背后的机制一直不明。病毒和宿主遗传因子,如nef缺失以及主要组织复合物等位基因,可部分解释这种差异性。然而,确定在病毒感染前的,抵抗HIV疾病进展的宿主免疫功能
5月30日,Sci. Transl. Med.杂志报道,科学家发现感染前免疫系统的组成对猿猴免疫缺陷病毒(SIV)感染后疾病的进展具有显著影响。这为HIV的研究提供了新的线索。
某些HIV患者对该病毒的抵抗性很强,而有些患者则进展迅速。其背后的机制一直不明。病毒和宿主遗传因子,如nef缺失以及主要组织复合物等位基因,可部分解释这种差异性。然而,确定在病毒感染前的,抵抗HIV疾病进展的宿主免疫功能一直存在难度。
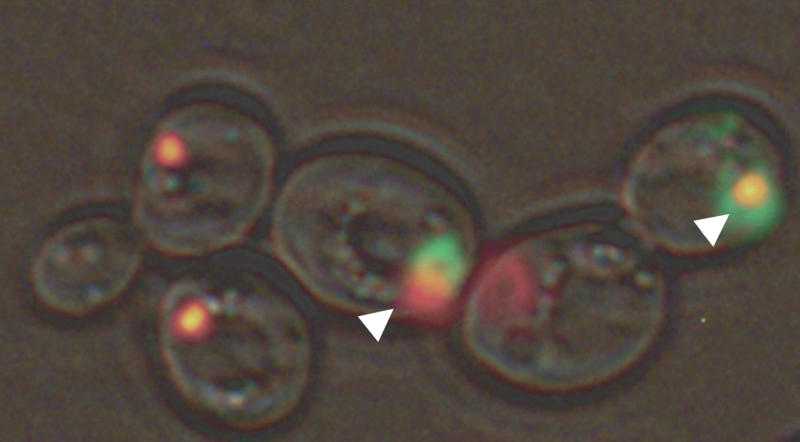
研究者发现,预先存在的辅助性T17细胞(TH17)种群大小控制着恒河猴体内的猿类免疫缺陷病毒的复制。在感染前,如果动物血液和肠道组织中TH17细胞的含量高,它们经历的最大及设定点病毒载荷将比TH17细胞的含量低的对照组动物低一个log单位。在感染前,给予恒河猴白介素-2和粒细胞集落刺激因子治疗,会导致TH17的消耗,并降低其与CD3+CD4+CD25+CD127low调节性T细胞之间的比率。这种治疗还会引起感染后持续6个月的高病毒载荷。
这些结果证实,HIV感染前宿主免疫系统的组成对感染后疾病的进程有影响。该研究为理解患者间对抗HIV治疗和疫苗的反应差异提供了新的研究框架。(生物谷bioon.com)

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
SIV Replication in the Infected Rhesus Macaque Is Limited by the Size of the Preexisting TH17 Cell Compartment
Dennis J. Hartigan-O’Connor1,*,?, Kristina Abel2,3,?, Koen K. A. Van Rompay3, Bittoo Kanwar1,4 and Joseph M. McCune
The mechanisms by which some HIV-infected subjects resist disease progression, whereas others progress rapidly, are incompletely understood. Viral and host genetic factors, such as nef deletions and major histocompatibility complex alleles, explain a portion of the observed variability. However, it has been difficult to identify host immune functions that may be present before infection and that allow resistance to lentiviral disease progression. Here, we show that simian immunodeficiency virus replication in the infected rhesus macaque is limited by the size of the preexisting T helper 17 (TH17) cell compartment: Animals with a high representation of such cells in blood and intestinal tissue before infection experienced peak and set-point viral loads about one log unit lower than those with a lower representation of TH17 cells. Reciprocally, treatment of macaques with interleukin-2 and granulocyte colony-stimulating factor before infection led to depletion of TH17 cells, reduction of the ratio between TH17 cells and CD3+CD4+CD25+CD127low regulatory T cells, and higher viral loads for 6 months after infection. These results demonstrate that the composition of the host immune system before infection has an influence on the course of disease after infection. Furthermore, to the extent that this influence shapes and interacts with T cell–mediated responses to virus, our findings provide a new framework for understanding interindividual variation in responses to therapies and vaccines against HIV.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Transl#
24
#疾病进展#
25
#TRA#
21
#Transl.#
29
#Med#
22