Dig Liver Dis: 功能性慢性水泻患者中粪钙卫蛋白水平可作为微观结肠炎的生物标志物
2020-03-14 MedSci原创 MedSci原创
目前关于使用粪便标志物来进行一些生物学标记的检查还比较少,本项研究旨在评估粪钙卫蛋白是否可以作为微观结肠炎的诊断标志物。
背景及目的: 目前关于使用粪便标志物来进行一些生物学标记的检查还比较少,本项研究旨在评估粪钙卫蛋白是否可以作为微观结肠炎的诊断标志物。
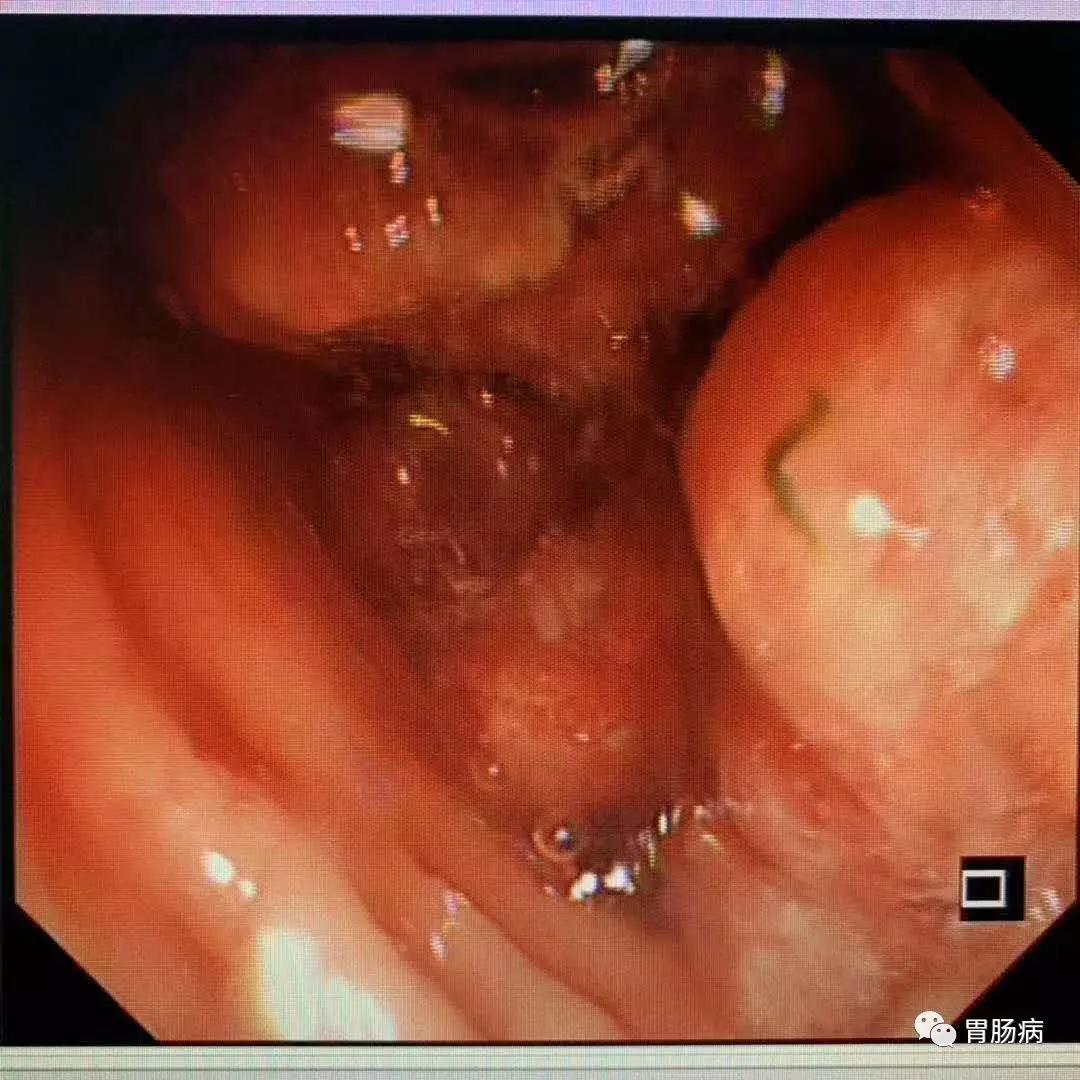
方法 研究人员对因慢性水样腹泻而满足功能性疾病标准的结肠镜检查患者进行评估。所有患者的结肠粘膜正常,或允许轻度红斑和浮肿。并检测分析粪便钙卫蛋白水平。使用逻辑回归分析来评估与粪便钙卫蛋白升高和微观结肠炎的诊断相关的变量。
结果 本项研究共包括94例患者,其中30例被诊断为微观结肠炎,64例为对照组。镜下结肠炎的钙卫蛋白水平中位数为175(IQR,59–325),对照组为28(IQR,16–111)(p <0.001)。粪钙卫蛋白的最佳临界值> 100μg/ g(AUC,0.73),敏感性为67%,特异性为75%。所用药物的数量≥3(OR,3.9;95%CI,1.4-10.4)和显微镜下结肠炎的诊断(OR,6;95%CI,2.2-16.3)与钙卫蛋白水平升高有关。年龄> 60岁(OR,3.8; CI,1.4-10.1)和钙卫蛋白水平(OR,5.3;95%CI,2-14.1)与患上微观结肠炎的风险有关。
结论 粪尿中钙卫蛋白的浓度升高经常在显微镜下的结肠炎中发现,可能有助于诊断60岁以上的慢性水样腹泻。
原始出处:
Lissette Batista. Et al. Usefulness of fecal calprotectin as a biomarker of microscopic colitis in a cohort of patients with chronic watery diarrhoea of functional characteristics. Digestive and Liver Disease. 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#功能性#
27
#标志物#
44
#Dis#
29
#生物标志#
26
#生物标志#
33