JACC:PCI术后合并分叉病变,常规支架与专用分叉支架如何选择?
2015-02-24 张旭栋 MedSci原创
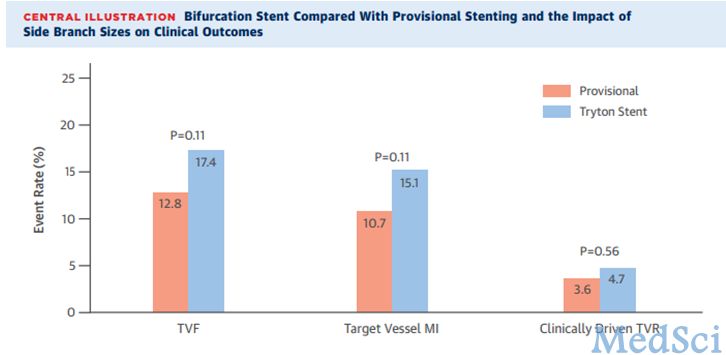
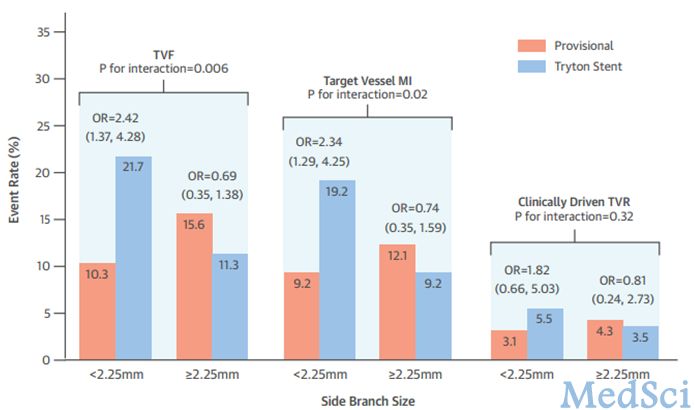
有症状的冠心病患者,在行径皮冠状动脉介入术后,经常会发生分叉病变,其比率接近15%-20%。尽管支架技术目前已经有了很大的进展,然而,分叉病变对于心脏疾病的介入治疗仍然是一项重大的挑战,其与围手术期心肌梗死,支架内血栓,远期再狭窄有着密切的联系。虽然已经有了很多对应的技术与治疗策略,目前的主流方案仍然是:主干病变首先治疗,分叉病变需要时再进行治疗。几项小的随机研究显示,对于
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
42
#PCI术#
34
很好,客观
114
#ACC#
33
#PCI术后#
33
#分叉病变#
34
不错的文章,学习了
96
明白了
99