Cell子刊:靶向作用休眠状态的HIV彻底攻克艾滋病
2016-09-21 佚名 生物谷
图片来源:medicalxpress.com 近日,来自蒙特利尔大学医院研究中心的研究人员通过对进行抗逆转录病毒疗法(ART)的HIV患者进行研究,开发了一种新型技术,该技术能够在患者机体中鉴别出HIV隐藏的罕见细胞,相关研究刊登于国际杂志Cell Host & Microbe上。 为何病毒会被唤醒?为了杀灭HIV,研究者们进行了多项研究来寻找HIV/AIDS的疗法,如今研究者们开
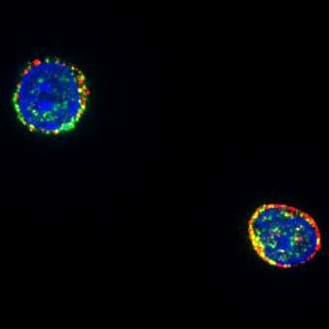
图片来源:medicalxpress.com
近日,来自蒙特利尔大学医院研究中心的研究人员通过对进行抗逆转录病毒疗法(ART)的HIV患者进行研究,开发了一种新型技术,该技术能够在患者机体中鉴别出HIV隐藏的罕见细胞,相关研究刊登于国际杂志Cell Host & Microbe上。
为何病毒会被唤醒?为了杀灭HIV,研究者们进行了多项研究来寻找HIV/AIDS的疗法,如今研究者们开发了一种能够检测隐藏HIV的罕见细胞的高精准技术,隐藏HIV的细胞能够有效阻断当前疗法对HIV的抑制和杀灭。研究者Kaufmann教授说道,我们能够“唤醒”病毒,并且在极低水平下(一百万个细胞中仅有一个)寻找隐藏病毒的细胞,这就达到了一种前所未有的准确度,同时该研究也为实时监测HIV阳性患者以及开发新型个体化疗法提供了一定帮助。
尽管患者进行了ART疗法治疗,但其机体的细胞和组织中依然会存在HIV病毒库,病毒库中持续存在的病毒大多会在CD4+ T淋巴细胞中生存并且复制,当抗逆转录病毒药物成功控制感染个体机体的HIV病毒载量,并且抑制感染个体进展为AIDS时,一些病毒会持续在感染者机体中存活数年,如果患者停止了疗法,隐藏的HIV就会被再度激活。CD4+ T淋巴细胞具有高度可变性,为了开发新型靶向性的疗法来消除这些残留的感染细胞,研究者们就需要准确知道病毒到底隐藏在CD4+ T淋巴细胞的哪些位置,本文研究就揭开了HIV的藏身之所,这样一来研究者就能够鉴别出隐藏HIV的细胞并且对这些细胞定量,随后再检测药物对HIV的作用效果。
研究者开发的这种检测病毒存储库的创新性技术的精确性是当前技术的1000倍,一旦病毒隐藏的场所被发现,研究者就能够利用一种“激活并杀死(shock and kill)”的策略来分两个阶段消除HIV,首先必需将HIV从休眠状态唤醒过来,其次病毒就会被免疫系统或靶向药物发现,并被消灭。文章中研究者Kaufmann的研究小组对30名HIV感染者进行研究,在患者开始疗法之前和接受ART疗法之后对患者的血液进行分析,随后研究者表示,他们在几乎所有患者的CD4+ T淋巴细胞中都检测到了HIV的存在。
随后研究人员检测了两种所谓的潜伏期逆转药物:苔藓抑素和巨大戟醇的衍生物,这两种药物都可以用来治疗癌症,但同时其还能被用于抵御HIV;研究者表示,但这项研究在实验室中进行时,他们或许就能够利用诸如上面的药物来激活病毒,同时患者还在继续进行ART疗法来确保被再度激活的病毒不会感染机体其它细胞。
研究者Baxter说道,在实验室研究中我们发现,苔藓抑素和巨大戟醇的衍生物两种药物能够够唤醒不同群体的CD4+ T淋巴细胞,随后唤醒不同的病毒存储库,巨大戟醇衍生物能够激活名为中枢记忆细胞的表达,这些记忆细胞能够在患者机体中存活数年,而其主要依赖于特殊HIV隐藏的场所。为了尽量减少病毒的存储,研究者必须对患者进行评估,并且利用激活并杀死的策略来治疗患者。
在对人体进行潜在的疗法试验之前,研究者计划利用猴子来进行试验,评估新型药物激活猴子机体相似HIV病毒库的效力,从而确定病毒隐藏的场所;如果药物具有良好的耐受性的话,研究者将会在几年后开展临床试验;经过30年治疗HIV感染和AIDS的漫漫长路之后,相信本文研究或为科学家们最终并且寻找HIV感染并且隐藏的细胞提供新的思路,也为科学家们开发唤醒并且有效杀灭HIV的靶向性疗法的开发提供一定的研究基础和帮助。
原始出处
Baxter AE1, Niessl J1, Fromentin R2, Richard J2, Porichis F3, Charlebois R2, Massanella M2, Brassard N2, Alsahafi N4, Delgado GG2, Routy JP5, Walker BD6, Finzi A4, Chomont N2, Kaufmann DE7.Single-Cell Characterization of Viral Translation-Competent Reservoirs in HIV-Infected Individuals.Cell Host & Microbe.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#休眠#
32
#Cell#
24
#CEL#
20
#靶向作用#
42