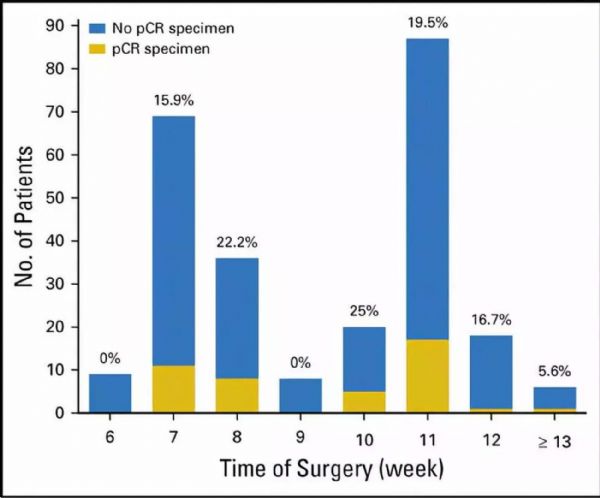
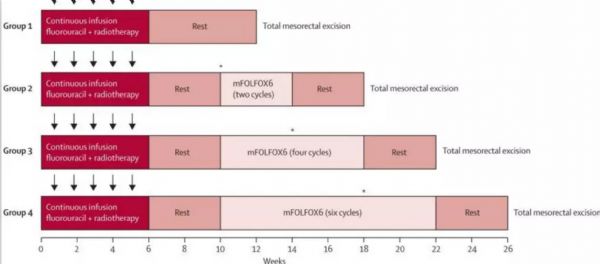
病例分析丨局部晚期直肠癌治疗,如何很大程度提高pCR率?
2018-07-16 杜丰 医学界肿瘤频道
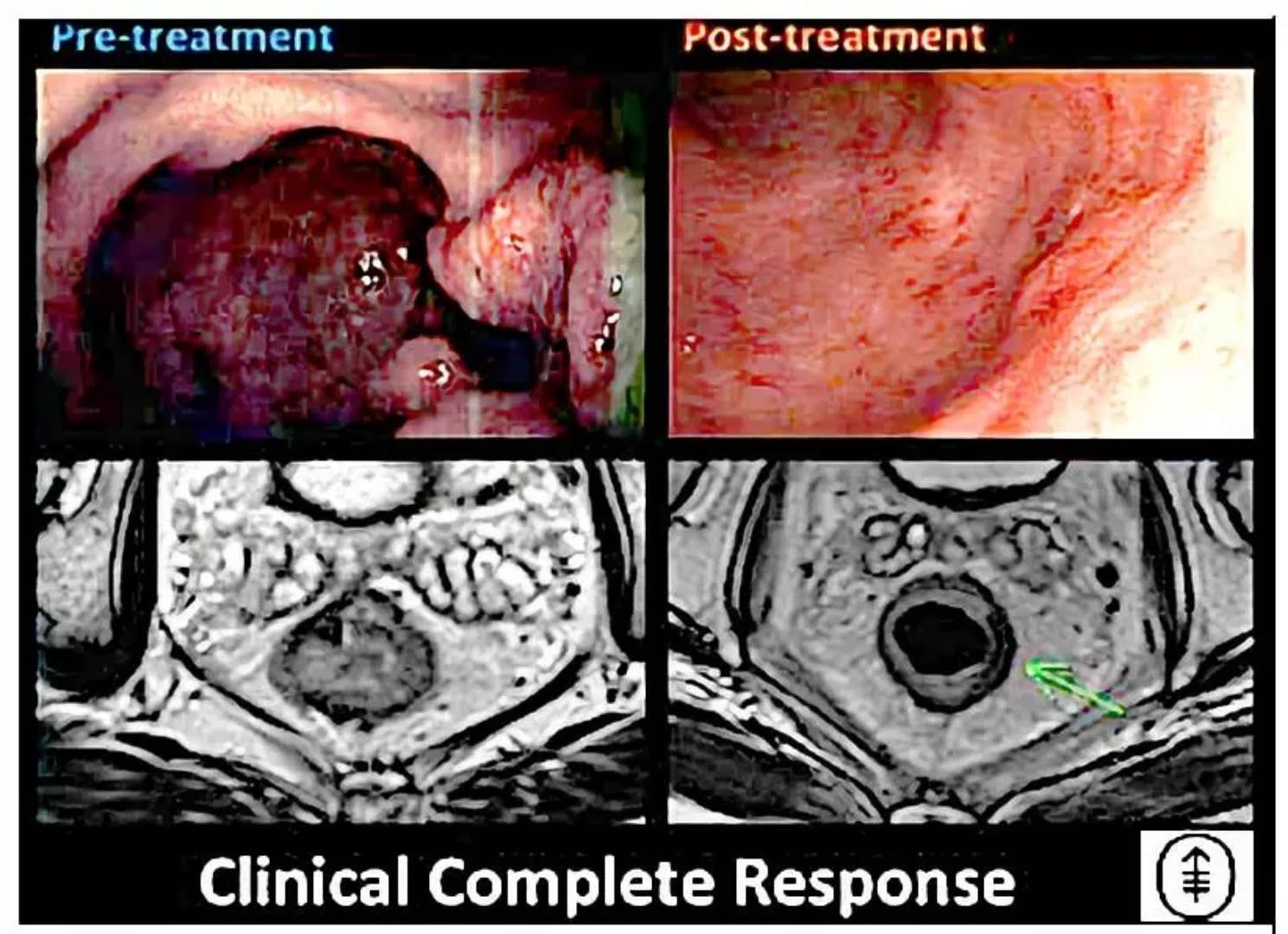
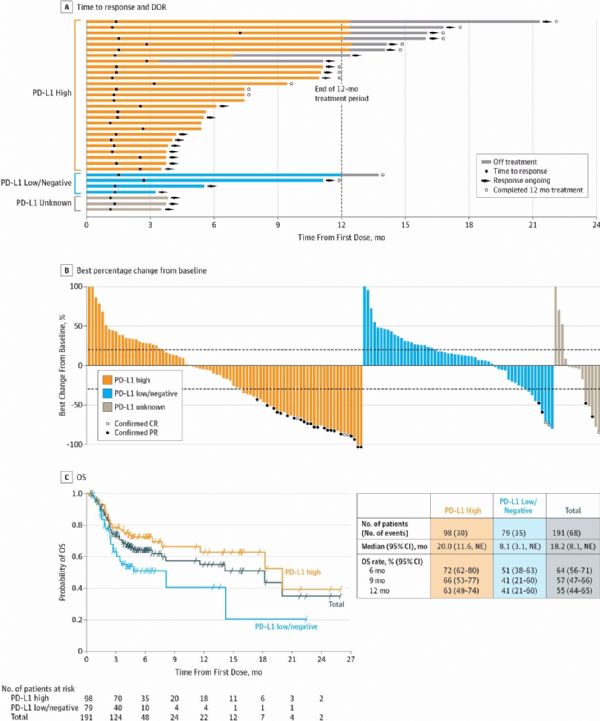
47岁女性,大便带血2月,肠镜示距肛门口5cm蕈伞状肿物,部分阻塞肠管。病理示中分化腺癌,微卫星状态稳定。盆腔CT及MRI见直肠周围脂肪间隙小淋巴结,肿瘤侵及直肠周围脂肪,未累及周围筋膜。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#局部晚期直肠癌#
32
#局部晚期#
30
#pCR率#
31
#局部#
37
#PCR#
34
优质资源.共同学习
75
还是没有讲透如何提高的可行性办法啊
71