
高血压、糖尿病、血脂异常、吸烟是导致心血管疾病的重要危险因素已为人们所熟知,但了解心率与心血管疾病关系的人可能就不多了。
早就有人报道,哺乳动物寿命长短与心率呈反比。哺乳动物一生的心率是固定的,心率越慢,寿命越长。一切哺乳动物,包括人的一生,消耗总能量都是预先由内在基因定好的, 就像电池能量是一定的一样,静息心率越快,耗能越多,寿命越短。
这里所说的心率是指静息心率,也就是清醒不活动的情况下心脏窦房结发出冲动引发的每分钟心跳次数(窦性心率)。
传统心率正常值为什么受到质疑
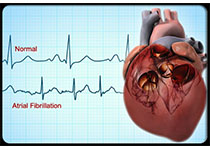
传统观点认为,窦性心率的正常范围为每分钟60~100次。随着研究的不断深入,人们逐渐发现心率与心血管疾病的预后具有密切关系,心率增快不仅是心血管疾病的独立致病因素,而且是心血管病患者死亡的强预测因子。
心率增快可导致血流动力学紊乱、血管顺应性下降、血管内皮功能受损以及炎症反应等,导致高血压、冠心病、糖尿病、肥胖等的发病率和死亡率增加。
在冠心病患者中,心率加快增加了心肌耗氧量、减少了冠状动脉血液供应,并可能诱发动脉粥样斑块破裂而增加心脏病发作的危险。持续性心动过速还可损害心功能,导致心动过速性心肌病。
相反,较慢的心率则更有利于对心肌缺血和心力衰竭的保护。因此,人们对传统心率的正常值范围提出了质疑。
心率每分钟80-100,提示心血管损害悄然进行
现在不少专家认为“正常心率”应该定义为每分钟55~80次,并将调控心率在正常范围作为开展心血管病早期预防的重要措施。
临床上大于每分钟100次的心率,容易引起患者和临床医生的重视,而每分钟80~100次之间的心率常被忽略或者不被重视,但是其对心血管的损害过程却在逐渐进行。
因此,有这种情况的朋友,应积极寻找引起心率增快的原因,如吸烟、过量饮酒、肥胖、糖尿病、睡眠不足、心理社会因素、植物神经功能紊乱、打呼噜(阻塞性睡眠呼吸暂停综合征)、慢性缺氧、不恰当使用药物、甲亢等,尽可能地去除诱因,以达到早期预防和控制的目的。
最佳心率为60-70,运动、药物让心率减慢
对于健康人来说,最佳心率是每分钟60~70 次。减慢心率最好的办法就是运动。长期耐力运动( 慢跑、走路、游泳) 增加副交感神经活性, 减低交感神经活性。
对于冠心病、慢性心力衰竭等心血管疾病患者,积极控制心率是一项有效、经济的治疗及预防措施。临床实践表明,只要无禁忌证,应用β受体阻滞剂类药物控制心率可以使冠心病患者心肌缺血发作减少,心肌梗死面积缩小,远期病死率降低。
对于不稳定型心绞痛、心肌梗死、慢性心力衰竭患者如能耐受可将静息心率控制到每分钟50~60次,伴有心房颤动者,应将静息心率控制于每分钟80次以下。
高血压患者除了平稳降压外,也应同时注意控制心率。除了β受体阻滞剂类,其它可在医生的指导下酌情选用(单用或联合应用)治疗药物,提高生活的质量。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










理学参考物
43
学习!
53
快
44
要吃药了
56
学习了
52