高龄心血管病患者中心血管危险因子的性别差异:PROTEGER研究
2012-01-01 MedSci原创 MedSci原创
回顾既往的临床研究结果,我们发现男性和女性虽然有着相似的心血管危险因子,但这些危险因子所导致心血管疾病在男女之间却并不相同。例如,男性更容易患有冠心病及心力衰竭,而女性则更易发生高血压和糖尿病。这提示我们,是否这些心血管危险因子在致病机制方面存在着一定的性别差异。此外,女性发生心血管疾病的时间往往要比男性晚10年左右,但在绝经后,女性的心血管疾病的患病率和死亡
回顾既往的临床研究结果,我们发现男性和女性虽然有着相似的心血管危险因子,但这些危险因子所导致心血管疾病在男女之间却并不相同。例如,男性更容易患有冠心病及心力衰竭,而女性则更易发生高血压和糖尿病。这提示我们,是否这些心血管危险因子在致病机制方面存在着一定的性别差异。此外,女性发生心血管疾病的时间往往要比男性晚10年左右,但在绝经后,女性的心血管疾病的患病率和死亡率会随着年龄的增长而逐渐上升。这往往被认为是由于失去了雌激素的心血管保护作用而引起的。如果真是如此,那么,在高龄的心血管疾病患者中,在绝经多年以后,心血管危险因子对死亡的预测价值应该可以在男女间表现出一致性的结果。为了验证这一假设,我们在PROTEGER人群中展开了有关心血管危险因子性别差异的研究。
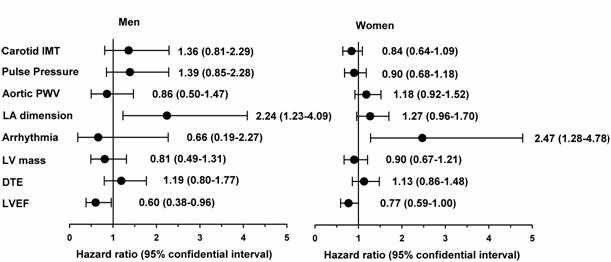
我们从法国巴黎的Charles Foix和Emile Roux两所医院的老年科募集了331名70岁以上的心血管疾病患者(其中86名男性,平均年龄86.8岁)。在经过了平均378天的随访,有110例患者死亡。我们利用超声技术检测了患者的颈动脉内中膜厚度(IMT),左心房内径(LAD),舒张早期二尖瓣血流的减速时间(DTE)和左心室射血分数(LVEF);利用心电图技术判断了患者是否患有心律失常;利用平面张力检测仪器测量了患者的脉搏波传导速度(PWV);利用常规的方法测量了患者的其它心血管危险因子(包括血压、年龄、体重指数、吸烟、血脂、血糖);同时研究这些危险因子与全因死亡之间的关系。结果发现,在完全矫正的模型中,我们发现,左心房内径增大(HR=2.24 per 1-SD; 95% CI: 1.23-4.09),左心室射血分数减少(LVEF,HR=0.60 per 1-SD; 95% CI: 0.38-0.96),总胆固醇与高密度脂蛋白的比值增加(HR=1.99 per 1-SD; 95% CI: 1.05-3.78)是男性患者全因死亡的显著预测因子;而在女性患者中,心律失常(HR=2.47; 95% CI: 1.28-4.78),血糖增高(HR=1.32 per 1-SD; 95% CI: 1.06-1.64),体重指数下降(HR=0.60 per 1-SD; 95% CI: 0.44-0.83)则可显著地预测全因死亡。
结论:
即使是在高龄的心血管疾病患者中,在女性绝经约20年以后,心血管危险因子在全因死亡的预测方面仍存在着显著的性别差异,并表现出与较年轻的人群相似的结果。该文发表于国际心血管杂志,2010年SCI影响因子6.8分(Int J Cardiol. 2011)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GER#
33
#中心血管#
28
#血管病#
27
#危险因子#
40
#高龄#
30
#PRO#
36
#心血管危险#
32