葛均波院士团队又有重大成果转化:有了TA,可以不用开胸换瓣啦~
2016-09-20 佚名 复旦大学附属中山医院微信公众号
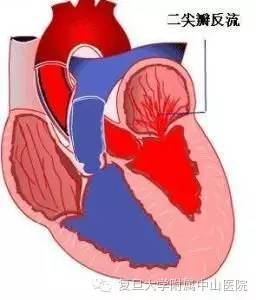
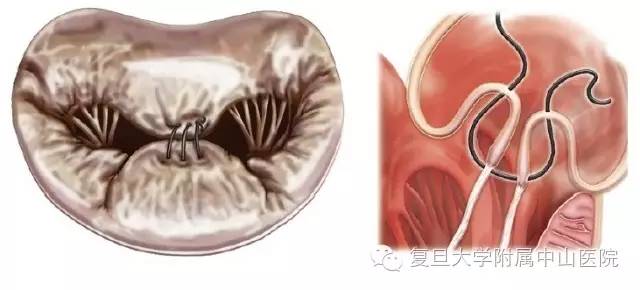
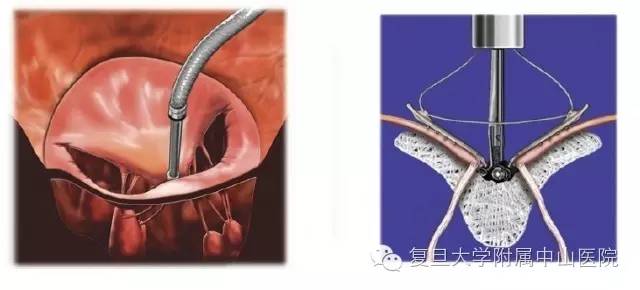
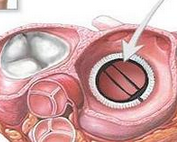
二尖瓣反流是最常见的心脏瓣膜疾病。上海复旦大学附属中山医院的葛均波院士团队最近发明了专治二尖瓣反流的瓣膜夹合器。对于二尖瓣反流患者来说,药物治疗只能改善患者症状,而不能延长患者生存或手术时机。所以,通常治疗它的方法:外科手术是首选!瓣膜修复或置换术被认为是该疾病的标准治疗方法,已被证实能缓解患者的症状及延长寿命。二尖瓣缘对缘修复的技术原理图只不过,外科手术创伤大,需要体外循环,许多高危患者不能耐受

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#成果转化#
33
医者丶匠者、心者向更高一层发展!
46
谢谢分享,继续学习。
54
好赞关心高兴
46
#葛均波院士#
38
与国外相比效果怎么样
59
真的很厉害
54
很好的技术,,
29
学习啦,,,
20
很好的内容,谢谢分享。
26