Oncologist:化疗难治性食管鳞状细胞癌患者使用apatinib(阿帕替尼)的疗效和安全性:II期临床研究
2021-11-29 yd2015 MedSci原创
研究表明,对于化疗难治性ESCC患者,原发性肿瘤得到控制,且没有严重侵犯气管、支气管或主要血管时,apatinib(阿帕替尼)有潜力成为一种有效且安全的治疗方法。
Apatinib(阿帕替尼)是一种小分子TKI,高度选择性地结合和强烈抑制VEGFR-2。先前的研究表明,阿帕替尼治疗可显著改善晚期胃癌患者的OS和PFS,且具有可接受的安全性。对于化疗难治性食管鳞状细胞癌(ESCC)患者,阿帕替尼的研究很少。因此,来自复旦大学团队开展了一项II期临床研究,评估化疗难治性食管癌患者使用apatinib(阿帕替尼)治疗的疗效和安全性。相关结果发表在Oncologist杂志上。

这是一项开放标签、单臂、II期临床研究(NCT03274011),纳入经一线或多线化疗后疾病进展的ESCC患者。入组标准为:经组织病理学证实的ESCC患者(年龄≥18岁),且对一种或以上化疗方案耐药(进展标准基于CT和MRI评估); ECOG评分为0-2;至少有一个可测量的病灶;以及血液,肝脏和肾脏功能正常。排除药物治疗血压未控制、有出血倾向或接受溶栓治疗或抗凝治疗的患者。
给药方案:所有患者持续接受阿帕替尼500 mg,每日1次,直到疾病进展、死亡、无法忍受的毒性或患者要求退出研究。允许剂量调整。在有≥3级不良事件的患者中,剂量降低到250mg。
主要研究终点是无进展生存期(PFS),次要研究终点是总生存期(OS)和客观缓解率(ORR)。
从2017年7月至2018年8月,研究中纳入40例化疗难治性ESCC患者。中位年龄为63岁(范围:47-76岁)。本研究中所有患者均未接受分子靶向治疗。72.5%(29/40)患者的ECOG评分为2。大多数患者在接受阿帕替尼前接受了治疗,其中57.5%(23/40)的患者在研究前接受了二线化疗,7.5%(3/40)的患者接受了三线化疗。21例(52.5%)患者曾接受原发肿瘤手术,而12.5%(5/40)患者的原发肿瘤未得到控制。复发或转移的主要部位为淋巴结(22%)、肺(40.0%)和肝脏(32.5%)。
数据采集于2019年11月6日结束。在研究期间,47.5%(19/40)的患者持续接受500 mg每日一次阿帕替尼,直到疾病进展或因任何原因死亡。47.5%(19/40)的患者有无法忍受的毒性,剂量降低到250 mg。40例患者中有7例(17.5%)在前2周停止了阿帕替尼治疗,52.5%(21/40)的患者减少剂量或停药。
40例患者中有37例患者可进行疗效评估。其中PR 3例,SD 23例,ORR为7.5%,DCR为65.0%。5%(2/40)的患者有明显的肿瘤坏死和肺转移空洞。当用mRECIST评估反应时,他们是PRs, ORR为12.5% (5/40)。
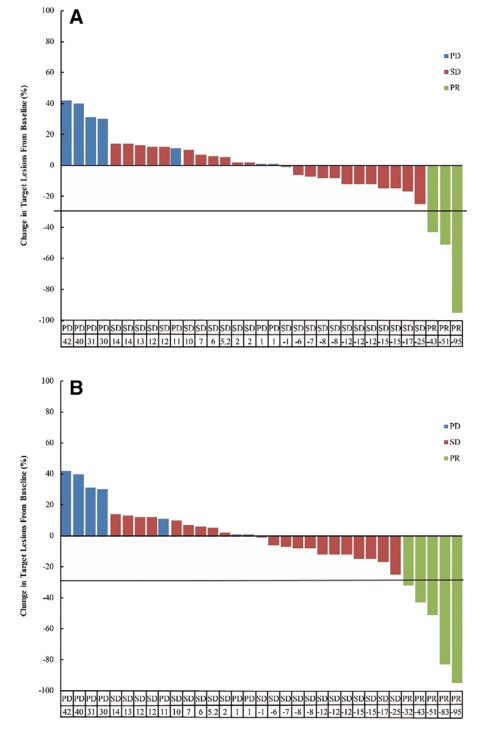
疗效评估
中位PFS为3.8个月(95% CI, 2.2 5.4),中位OS为5.8个月(95% CI, 3.2 8.4)。2个月时PFS率为60.4%,3个月时PFS率为57.7%。6个月OS率为45.0%,12个月OS率为15.9%。2例严重致死性支气管肺出血和1例食管瘘发生于原发肿瘤未控制患者(3/ 5,60%)。我们进行了排除不受控制的原发肿瘤患者的分析时,ORR和DCR分别为8.6%(3/35)和68.6% (24/35),mPFS2为3.9个月(95% CI, 3.3 4.5), mOS2为6.0个月(95% CI, 3.3 8.7)。2个月PFS2率为64.5%,3个月时为61.4%。6个月OS2率为47.2%,12个月OS2率为14.8%。
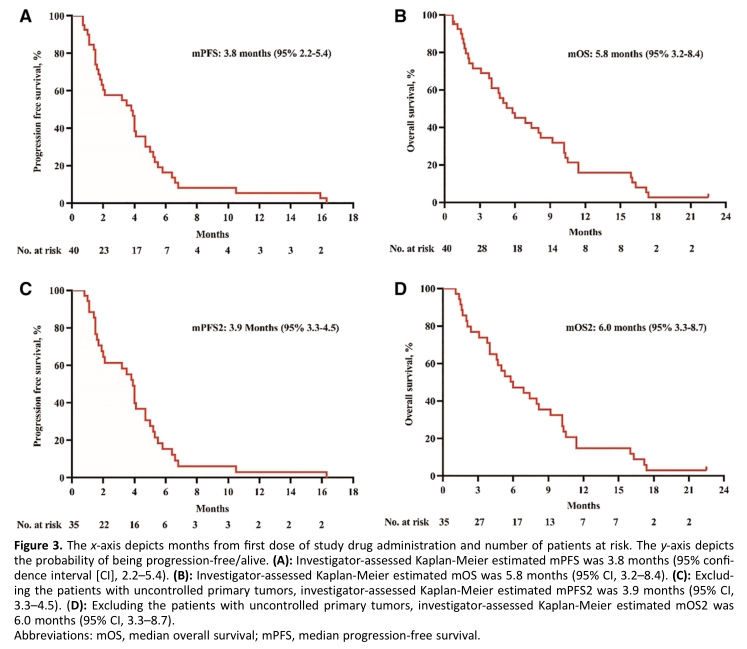
PFS和OS
常见的不良反应为疲劳(15%)、高血压(12.5%)和手足综合征综合症(10%)。2例因支气管肺大出血死亡,2例发生食管瘘。值得注意的是,两个食管瘘患者和一例大量致命性支气管肺出血的患者都是原发肿瘤未控制患者(3/5,60%)。第二例致命的支气管肺出血与大血管侵犯有关。
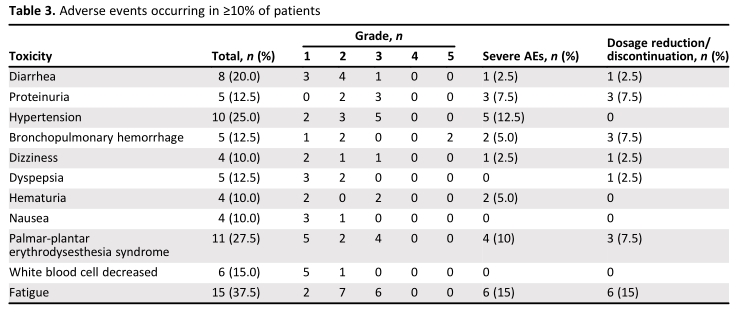
常见不良反应
综上,研究表明,对于化疗难治性ESCC患者,原发性肿瘤得到控制,且没有严重侵犯气管、支气管或主要血管时,apatinib(阿帕替尼)有潜力成为一种有效且安全的治疗方法。
原始出处:
Chu L, Chen Y, Liu Q, Liang F, Wang S, Liu Q, Yu H, Wu X, Zhang J, Deng J, Ai D, Zhu Z, Nie Y, Zhao K. A Phase II Study of Apatinib in Patients with Chemotherapy-Refractory Esophageal Squamous Cell Carcinoma (ESO-Shanghai 11). Oncologist. 2021 Jun;26(6):e925-e935. doi: 10.1002/onco.13668. Epub 2021 Feb 1. PMID: 33393167; PMCID: PMC8176978.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#细胞癌#
33
#I期临床#
35
#II期临床研究#
43
#Oncol#
44
#疗效和安全性#
25
学习了,谢谢分享
47
#APA#
43
#食管鳞状细胞癌#
42
#食管#
28
#GIST#
35