Neurology:接受血管内治疗(EVT)的急性脑卒中(AIS)患者中,活动性癌症患者在90天功能预后更差!
2022-02-12 Naomi MedSci原创
近日,有研究人员试图比较接受血管内治疗(EVT)治疗的急性脑卒中(AIS)患者和活动性癌症患者的临床、影像学和安全性结果。研究发现,在接受EVT治疗的AIS患者中,活动性癌症患者在90天功能预后更差。
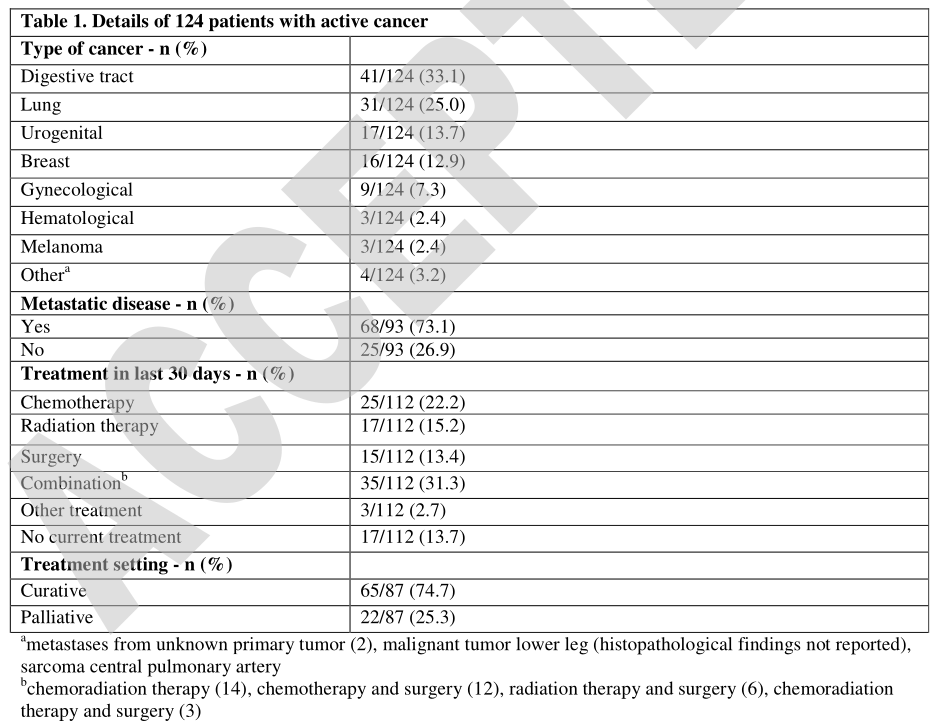
癌症患者发生急性缺血性卒中(AIS)的风险增加,特别是在诊断后的第1个月。卒中风险因癌症类型而异,一般在疾病的晚期和腺癌患者卒中风险较高。大约10% 的AIS患者已知患有癌症,3%-5% 的患者在卒中后2年内被诊断患有癌症。AIS患者最常见的癌症类型与大众相若(即肺癌、消化道癌及乳腺癌)。
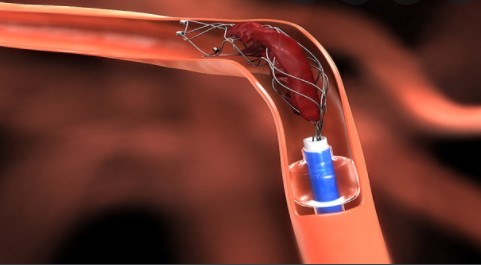
先前的研究发现,共病癌症与卒中严重程度增加、卒中进展和功能不良结局相关。此外,与非癌症患者相比,这些患者卒中复发的风险高出2-3倍。血管内治疗(EVT)通常是AIS患者唯一可能的治疗方法,因为癌症患者通常有静脉溶栓(IVT)禁忌症,如近期手术或凝血障碍。然而,除了病例系列研究和小规模的单中心研究外,关于卒中癌症患者EVT后的短期和长期预后的数据非常少。
近日,有研究人员试图探讨接受EVT治疗的AIS患者和活动性癌症患者的临床、影像学和安全性预后差异。
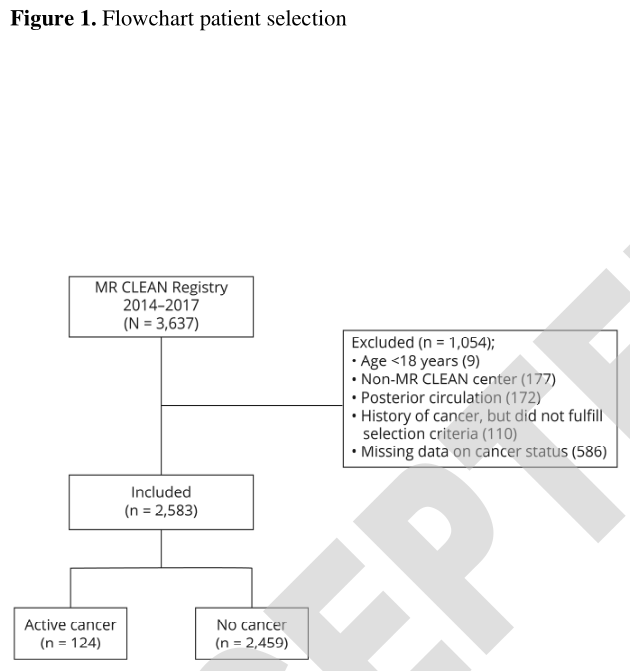
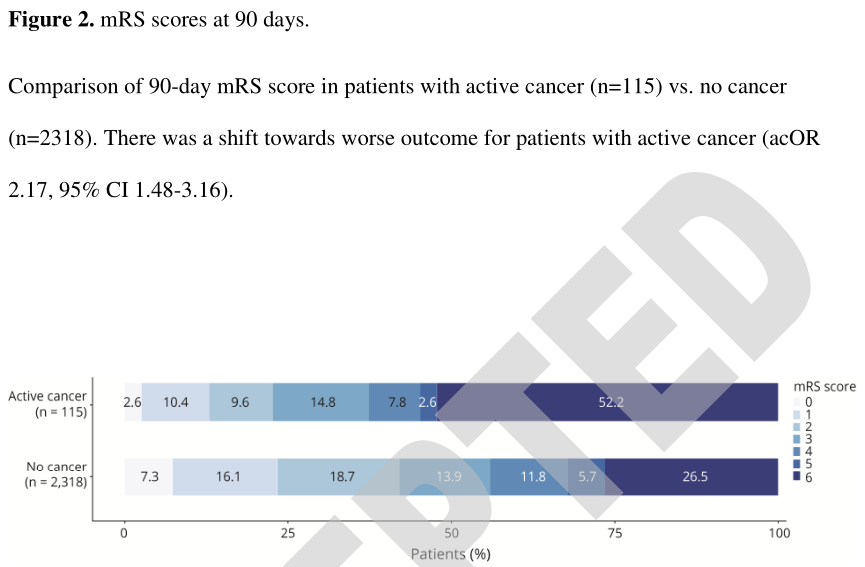
使用来自MR CLEAN Registry处的数据,将活动性癌症患者(定义为卒中前12个月内确诊的癌症、转移性疾病或目前接受癌症治疗)与非癌症患者进行比较。预后指标为90天修改 Rankin 量表(mRS)评分、死亡率、再灌注成功率(ETICI 评分≥2 b)、症状性颅内出血(SICH)和复发性卒中。亚组分析的患者进行了卒中前mRS评分为0或1和根据治疗设置(治愈或姑息)。分析根据预测变量进行调整。
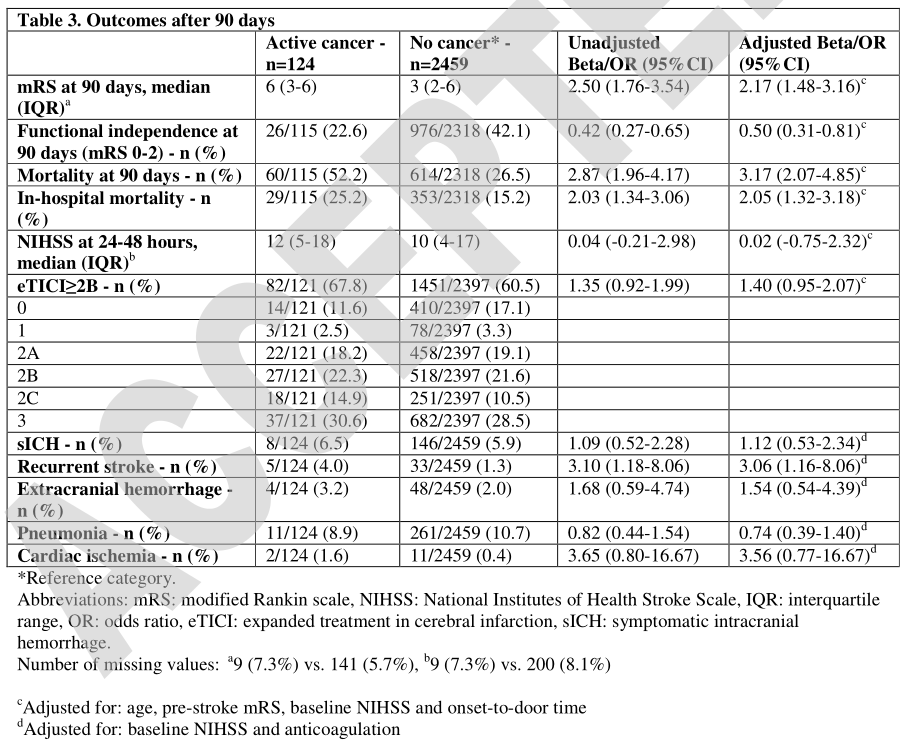
- 2583例接受EVT治疗的患者中,124例(4.8%)为活动性癌。他们更常出现卒中前残疾(mRS ≥2:34.1% 对16.6%),其中25.3% 的患者采用姑息治疗。
- 活动期癌症患者90天时功能转归趋于恶化(调整后的常见或2.2,95% CI 为1.5-3.2)。
- 在90天时,活动期癌症患者的独立性较差(mRS 0-2:22.6% vs. 42.0%,aOR 0.5, 95% CI 0.3-0.8) ,死亡率更高(52.2% 对26.5%,aor 3.2,95% CI 2.1-4.9)。再灌注成功率(67.8% 对60.5% ,aor 1.4,95% CI 1.0-2.1)与 SICH 率(6.5% 对5.9%,aor 1.1,95% CI 0.5-2.3)无差异。
- 90天内复发性卒中在活动期癌症患者中更为常见(4.0% 对1.3% ,aor 3.1,95% CI 1.2-8.1),卒中前期患者的敏感度分析显示,活动期癌症患者在90天后仍有更糟糕的结果(acor 1.9,95% CI 1.2-3.0)。
- 在姑息治疗环境中的活动性癌症患者恢复功能独立性的机会比在治疗环境中的患者少(18.2% 对32.1%),死亡率也较高(81.8%对39.3%)。
尽管在技术上取得了类似的成功,活动性癌症患者在进行EVT治疗后,其预后明显较差。此外,他们有复发性卒中的风险增加。然而,大约四分之一的患者恢复了功能独立,其他并发症的风险,尤其是 SICH,并没有增加。
这项研究提供了第Ⅰ类证据,活动性癌症患者接受EVT治疗的AIS在90天的功能预后比那些没有活动性癌症的患者更差。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#AIS#
48
#活动性#
42
#Neurol#
39
学习
59
学校
65
ffgggg
49
学习学习
68
认真学习了
73
希望能给癌症患者带来好的效果
58
#癌症患者#
27