Front Med:进行性纤维化间质性肺病 (PF-ILD) 的管理
2021-11-10 刘少飞 MedSci原创
进行性纤维化间质性肺病 (PF-ILD) 由多种间质性肺病 (ILD) 组成。肺移植是唯一的治愈性疗法,适合且有兴趣的患者可以考虑。支持性护理、适当的氧疗以及合并症的治疗是PF-ILD管理重要方法。

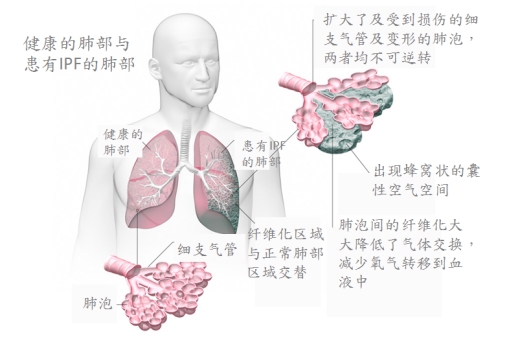
特发性肺纤维化 (IPF) 是典型的进行性纤维化间质性肺病 (ILD),其特征是呼吸衰竭加速、疾病频繁恶化和早期死亡。尽管非 IPF 纤维化 ILD 的结果通常更好,但有些人会发展出类似于 IPF 的进行性表型。这种进行性纤维化间质性肺病 (PF-ILD) 表型见于结缔组织病(如类风湿性关节炎、硬皮病、皮肌炎/多肌炎)相关的 ILD (CTD-ILD)、纤维化过敏性肺炎 (fHP)、尘肺病(如石棉, 矽肺)、结节病、特发性非特异性间质性肺炎 (NSIP) 和无法分类的 ILD。进展的危险因素包括年龄较大、男性、较低的基线肺功能以及放射学蜂窝状或常见的间质性肺炎 (UIP) 损伤模式。不管疾病触发,PF-ILD 通过自我维持失调的细胞修复、成纤维细胞增殖和肺泡功能障碍的机制进展,这些机制可以作为类似的目标。
药物疗法-抗纤维化疗法
尼达尼布是一种口服细胞内酪氨酸激酶抑制剂,可阻断参与纤维化进程的细胞信号通路。尼达尼布每天两次服用 150 毫克,可减少 IPF、硬皮病相关肺纤维化和最近的非 IPF 进行性肺纤维化个体用力肺活量 (FVC) 的下降。腹泻是尼达尼布最常见的副作用,发生在 60-76% 的个体中。可根据需要使用包含在药物泡罩包装中的止泻剂。
吡非尼酮是另一种口服抗纤维化药物,可通过抑制胶原合成和成纤维细胞增殖来减少纤维化进展。吡非尼酮减缓 IPF和无法分类的进行性纤维化 ILD的 FVC 下降。值得注意的是,由于不可预见的测量变异性,后一项研究没有达到其家庭肺活量测定的主要终点,并利用了临床肺活量测定的次要终点。吡非尼酮每天给药 3 次 (TID),为期 2 周,但如果出现症状,剂量可以以较慢的速度递增。常见的副作用包括恶心、呕吐、厌食和皮疹。胃肠道症状可以通过止吐药、抗酸剂和充足的膳食来改善。
Tocilizumab 是一种白细胞介素 6 信号传导抑制剂,也具有抗纤维化作用,并且最近被证明可以在系统性硬化症相关 ILD 中保留 FVC,作为focuSSced试验的次要终点,导致其获得 FDA 批准用于治疗硬皮病相关的 ILD。
免疫抑制
免疫抑制虽然用于 CTD 和 fHP,但对 IPF 有害,应避免。随着抗原回避,系统性口服皮质类固醇是有效的非纤维化HP和FHP。然而,最近的数据显示皮质类固醇可能不会改善 fHP 的死亡率或肺功能。对于使用皮质类固醇的 fHP 患者,过渡到硫唑嘌呤或吗替麦考酚酯可以改善副作用并稳定肺功能。
胃食管反流管理
胃食管反流在 IPF和结缔组织病相关 ILD中很常见,并且可能导致疾病进展。目前的指南推荐在 IPF 中进行抗酸治疗,但证据质量较低 。在回顾性研究中,抗酸剂减少了 IPF 的恶化和肺功能下降并提高了生存率。
肺动脉高压疗法
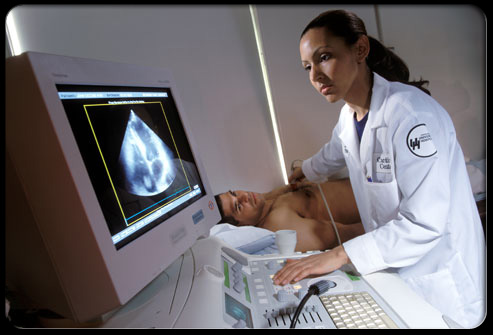
世界卫生组织(WHO)第3组肺动脉高压(PH)与ILD,并与更坏的症状和运动耐受力,早期死亡率,并增加了补充氧气需要相关。超声心动图显示右心室收缩压 (RVSP) 升高或右心功能障碍,应立即调查合并低氧血症或阻塞性睡眠呼吸暂停 (OSA)。
非药物疗法-支持性护理
应鼓励并为 PF-ILD 患者接种肺炎球菌、流感和 COVID-19 疫苗。间歇性缺氧可能导致肺纤维化的发展。应为静息饱和度或劳力性去饱和度≤ 88%的个体开具氧疗,因为它可以改善运动耐力和劳力性呼吸困难。夜间血氧饱和度测定也应进行,因为最大的睡眠饱和度会超过劳力性去饱和度并恶化结果。
肺移植
ILD是肺移植的最常见适应证,和移植已显示出延长生存期和改善症状中PF-ILD。移植后存活率逐年提高,最新数据显示 1 年存活率为 88.8%,5年存活率为 59.2%。然而,由于年龄较大和合并症,ILD 患者的存活率通常较低。对于合适的患者,应尽早讨论转诊到肺移植中心的问题,因为一旦列出,等待移植的中位时间约为 3 个月。
姑息治疗
尽管采用了目前的治疗方法,但许多 PF-ILD 患者进展时伴随着显着的临终症状负担。使用阿片类药物或苯二氮卓类药物可以安全地治疗致残性呼吸困难。咳嗽的治疗具有挑战性,应侧重于优化其他相关疾病过程。应尽早讨论临终关怀,以避免不符合患者偏好的疗法。早期参与综合姑息治疗可能会减少临终住院治疗,并允许在家中更有尊严地死亡。
未来方向
在过去的 10 年中,IPF 和其他 PF-ILD 的治疗取得了重大进展。尼达尼布、肺康复和适当的氧疗应用于患有进行性纤维化疾病的个体。肺移植应考虑在感兴趣的合适候选人中进行。吸入曲前列环素可用于 WHO 3 组 PH 和功能状态受损的个体,尽管进行了标准治疗。需要更多的研究来确定吡非尼酮、免疫抑制和抗酸治疗在全因和 PF-ILD 亚群中的疗效。
文献出处:
Copeland CR, Lancaster LH. Management of Progressive Fibrosing Interstitial Lung Diseases (PF-ILD). Front Med (Lausanne). 2021 Oct 13;8:743977. doi: 10.3389/fmed.2021.743977. PMID: 34722582; PMCID: PMC8548364.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肺病#
44
#进行性纤维化#
32
#ILD#
24
#纤维化间质性肺病#
44
#进行性#
41
#间质性#
0
#Med#
28