左室声学造影的临床应用
2015-01-30 南方医科大学附属南方医院 吴爵非 刘俭 查道刚 刘伊丽 中国医学论坛报
医学影像技术是20世纪医学研究取得重大成就的领域之一,其发展的核心内容是应用各种造影剂对比显像。超声造影是临床应用最广泛、也是唯一非常规应用造影剂的影像技术。本文将介绍在心血管疾病临床治疗中左室声学造影(LVO)的应用。 在LVO中,受试者经周围静脉注射超声造影剂(包裹1μm~10μm惰性气体的脂质或白蛋白微泡)。微泡通过肺血管床后进入左室,使左室影像对比增强,清晰界定左室壁内膜,以辅助观察
医学影像技术是20世纪医学研究取得重大成就的领域之一,其发展的核心内容是应用各种造影剂对比显像。超声造影是临床应用最广泛、也是唯一非常规应用造影剂的影像技术。本文将介绍在心血管疾病临床治疗中左室声学造影(LVO)的应用。
在LVO中,受试者经周围静脉注射超声造影剂(包裹1μm~10μm惰性气体的脂质或白蛋白微泡)。微泡通过肺血管床后进入左室,使左室影像对比增强,清晰界定左室壁内膜,以辅助观察室壁运动和室壁结构改变。
LVO在负荷超声试验中的应用
国际指南明确指出,可疑稳定性冠心病(SCAD)患者,如验前概率[PTP,根据年龄、性别和胸痛类型预测患冠心病(CAD)的可能性]为15%~65%,就应进行心脏负荷试验,评估冠脉血流储备和检出缺血心肌,进而确定后续诊疗方案。
心电图(ECG)运动负荷(平板或踏车运动)试验仍是最基本的心脏负荷试验。但ECG运动负荷试验对存在左束支传导阻滞(LBBB)、起搏心律和预激综合征(WPW)等的患者缺乏诊断价值。同时,ECG运动负荷试验的假阳性结果常见于有左室肥厚、电解质紊乱、室内传导异常、心房颤动和应用洋地黄的患者。此外,ECG运动负荷试验在女性患者中的敏感性和特异性较低。
因此,在ECG运动负荷试验的基础上,国际广泛开展了无创性负荷影像试验,从负荷后的室壁运动和心肌血流灌注变化来检出可逆性心肌缺血。其中负荷超声和负荷核素[单光子发射计算机断层显像(SPECT)]是最常用的手段。与其他影像试验相比,运动负荷超声的室壁运动分析对SCAD诊断的敏感性、特异性较高。
各个标准二维(2D)左室超声切面均与冠状动脉各个主支分布密切相关,这是应用负荷超声试验的基础。发现负荷后某个左室室壁节段增厚异常(供-求不匹配),可推测相应冠脉的狭窄程度。因此,超声图像的清晰度直接影响结果评估的质量。2013年欧洲心脏病学会(ESC)SCAD指南明确提出,当静息超声显示有2个以上连续左室节段不清楚时就应常规应用超声造影剂。
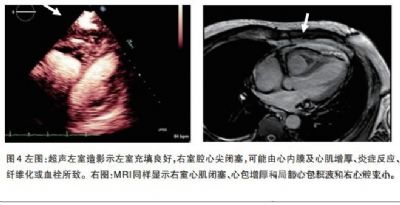
2014年,我们对100余例患者进行了联合平板运动负荷超声和ECG检查,均安全、高质量地完成,与大家分享几例。

图2冠脉造影提示LAD病变及置入冠脉支架前后FFR测量结果。A:LAD狭窄处术前FFR测值为0.72;B:LAD狭窄处支架置入术后FFR为0.85。
图2 为1例男性患者,1个月前因急性下壁ST段抬高型心肌梗死,在某医院行右冠状动脉(RCA)支架重建,同时发现LAD病变,嘱择期处理。平板负荷超声试验检出左室前壁心肌缺血。冠脉造影显示LAD中重度狭窄。LAD灌注心肌区域的血流储备分数(FFR)为0.72(FFR小于0.75~0.80是进行血流重建的指征)。置入支架后,FFR恢复至0.88。
LVO用于特殊心肌病的诊断
图3为1例男性患者,52岁,反复心力衰竭史5年。2013年经某医院心脏超声检查显示双房增大,左室射血分数(LVEF)为31%,诊断为限制型心肌病。同年该院心脏磁共振成像(MRI)显示全心增大、室间隔及左室壁广泛延迟强化(LGE),诊断为扩张型心肌病。2014年6月28日经我院心内科经胸超声检查显示双房大、右室大、重度三尖瓣关闭不全、肺动脉压38mmHg、LVEF为43%。因超声图像欠清晰,遂进行LVO,结果显示为典型左室心肌致密化不全。
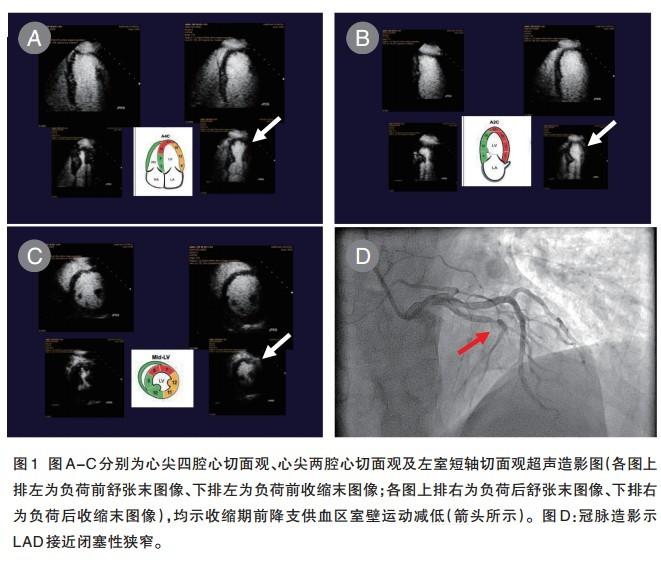
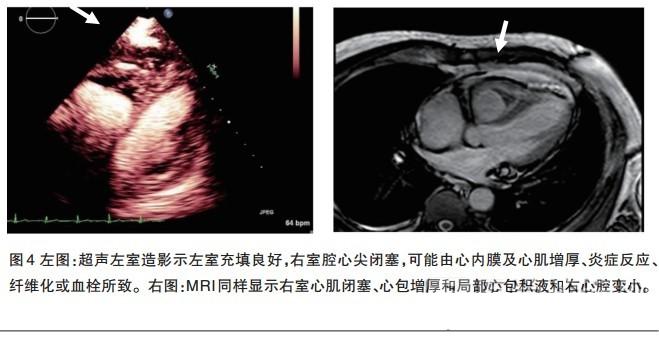
图4为1例60岁男性患者,因眼睑及下肢浮肿1月余来我院检查。ECG显示有轻度ST-T改变。因经胸超声图像不够清晰而行超声LVO,意外发现右室心尖闭塞,考虑为限制型心肌病。结合多年血嗜酸性粒细胞增高史,推断为少见的嗜酸性粒细胞增多性心内膜心肌病(Loffler’s心肌病)。遂行心脏MRI检查,显示为右室心尖内膜增厚、心肌纤维化、心包增厚、右室变小、右房增大。测周围静脉压为17cm水柱。右心心内膜活检显示,嗜酸性粒细胞局部沉积;骨髓活检显示,各阶段嗜酸性粒细胞增多。经泼尼松口服治疗,嗜酸性粒细胞值恢复正常。最后诊断为特发性嗜酸性粒细胞增多性心内膜心肌炎、右室限制型心肌病、轻度大循环淤血。
无创负荷试验室应为心内科的主要组成单元之一,用于筛查CAD、冠脉重建后心肌功能评估和非心脏手术前CAD评估。心电图运动负荷试验是最基本的无创手段,运动/药物影像负荷试验是必要的补充手段(尤其针对女性患者)。负荷SPECT是最常用的评估心肌灌注方法,负荷超声是最常用的评估室壁运动方法,同步左室声学造影能提高室壁运动分析的质量和可信度,且对特殊心肌病有特异性诊断价值。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#声学造影#
30
#临床应用#
30
非常好的文章,学习
78
已阅
81
明白
137
#造影#
33