Cell Research:环装RNA编码蛋白的重要机制
2017-03-16 上海生命科学研究院 上海生命科学研究院
3月10,中国科学院-马普学会计算生物学伙伴研究所研究员王泽峰在《细胞研究》(Cell Research)上在线发表了题为Extensive translation of circular RNAs driven by N6-methyladenosine 的研究论文,该研究发现了大量的环形RNA可作为信使RNA来编码蛋白,这些环形信使RNA通过一种常见的RNA甲基化修饰m
3月10,中国科学院-马普学会计算生物学伙伴研究所研究员王泽峰在《细胞研究》(Cell Research)上在线发表了题为Extensive translation of circular RNAs driven by N6-methyladenosine 的研究论文,该研究发现了大量的环形RNA可作为信使RNA来编码蛋白,这些环形信使RNA通过一种常见的RNA甲基化修饰m6A,来驱动非帽依赖性的翻译机制来合成蛋白质。该研究进一步拓展了环装RNA的功能,对蛋白质来源的多样性有新的认识,具有十分重要的理论意义。
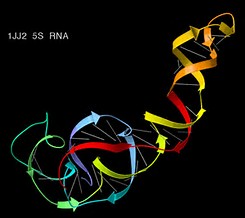
环状RNA在某些病毒中普遍存在,然而近年才在真核生物中发现大量这种非主流RNA。人类的环状RNA主要是由外显子的反向剪接产生的,但关于其生物功能尚无定论。先前研究显示,环状RNA是一种非编码RNA,可以如同海绵一样吸附miRNA或RNA结合蛋白,从而起到调控基因表达的作用。
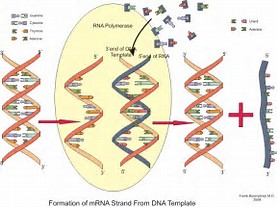
人的细胞中所有的已知mRNA都含有5'端帽结构,这一帽结构是大部分mRNA翻译所必需的。然而在一些特殊情况如细胞应激条件下,有些mRNA可以不依赖于帽结构而靠一个叫IRSE的顺式调控原件从mRNA的中间启动翻译。这种IRES驱动的蛋白翻译在RNA病毒中很常见,但只在一小部分的真核细胞mRNA中发现。在王泽峰组的前期工作中,他们发现插有IRES的编码GFP的环状RNA可以在细胞中被翻译。而新的工作中,他们发现环状RNA中富含m6A甲基化修饰,而且这些碱基修饰可以像IRES一样驱动环状RNA翻译。王泽峰认为,"这两个发现放在一起,就可推断出有大量的环状RNA被翻译成蛋白质这一令人惊讶的结论,说明人的细胞中存在有大量的环状RNA编码的未知蛋白。"这是一个很令人兴奋的结论,说明人类蛋白质的多样性远比从前想的大。
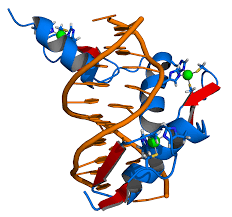
该文作者们进一步研究了环形RNA的翻译机制,发现了m6A识别蛋白YTHDF3能够结合到环状RNA的修饰位点并募集eIF4G2和其他翻译起始因子来驱动环状RNA的翻译。同时,他们通过多核糖体分析和RNA测序发现大量的环状RNA与多核糖体结合在一起。在此基础上,利用质谱分析的方法鉴定了一些由环状RNA反向剪接接口编码的新肽段。
尽管不排除很多环状RNA仍可能是非编码RNA,但新结果证明其中一大部分可以像信使RNA一样翻译成蛋白。"这一发现模糊了编码和非编码RNA的界定。"王泽峰认为,"信使RNA不见得一定需要是线性的,环状RNA显然是一类新的信使RNA。"
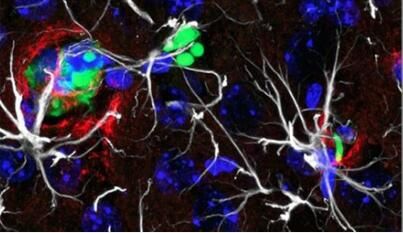
新文章尚未解答的重要问题是这些环状RNA编码的蛋白功能是什么,但他们提出了一些有趣的可能性。正常情况下,真核细胞中蛋白质合成的主要方式是通过5'端帽依赖性翻译,但在应激环境下或一些癌症中,5'端帽依赖性翻译会被抑制而非帽依赖性翻译将会取代。因为环状RNA没有5'端帽结构,所以所有的环状RNA翻译都是通过非5'端帽依赖性翻译进行的。因而环状RNA可能通过产生刺激诱导蛋白在细胞应激反应中发挥重要作用。根据类似推理,环状RNA编码的蛋白可能在癌症发展过程中发挥重要作用。
此项研究和之前的研究都表明m6A可以像IRES一样启动翻译,而在信使RNA中存在大量的m6A修饰。因此王泽峰相信:"类似于一个基因可以通过可变剪接产生多个信使RNA异构体一样,一个信使RNA可能通过非帽依赖性翻译产生多种蛋白质。"
参与此项工作的合作者包括来自浙江大学、中科院上海生命科学研究院生物化学与细胞生物学研究所、华东理工大学和大连医科大学的科学家。
原始出处:
Yang Y, Fan X, Mao M,et al. Extensive translation of circular RNAs driven by N6-methyladenosine.Cell Res. 2017 Mar 10.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
26
#Cell#
29
#Research#
32
#编码#
26
lncRNA是热点,但不见得是靶点,尤其是药物靶点
59