Int J Cancer:前列腺癌细胞中GRB10通过与PP2A互作维持AR活性
2020-10-31 AlexYang MedSci原创
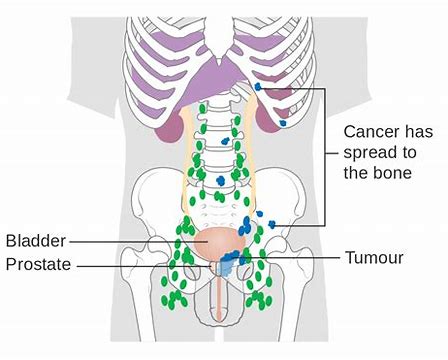
雄激素受体(AR)信号能够驱动前列腺癌(PCa)进展是。不幸的是,雄激素阻断疗法和使用更强效的AR途径抑制剂(ARPIs)并不能起到治愈效果。ARPI耐药(如去势抵抗性PCa,CRPC)将不可避免地发
雄激素受体(AR)信号能够驱动前列腺癌(PCa)进展是。不幸的是,雄激素阻断疗法和使用更强效的AR途径抑制剂(ARPIs)并不能起到治愈效果。ARPI耐药(如去势抵抗性PCa,CRPC)将不可避免地发展。
之前,研究人员证明了GRB10是一个AR转录抑制基因,在功能上有助于CRPC的发展和ARPI耐药。在患者来源的异种移植模型中,研究发现GRB10的表达在CRPC发展前升高,并在临床CRPC样本中显著上调。最近,有研究人员分析了GRB10敲除的PCa细胞的转录组数据,发现AR信号下调。虽然GRB10敲除后AR靶基因的mRNA表达下降,但AR的表达在mRNA或蛋白水平上没有受到影响。进一步研究发现,对AR转录活性至关重要的AR丝氨酸81(S81)的磷酸化水平在GRB10敲除后降低,而过度表达后则增加。GRB10基因敲除细胞的荧光素酶测定也表明AR活性降低。免疫沉淀结合质谱法发现GRB10与PP2A复合物之间存在相互作用,PP2A复合物是已知的AR磷酸酶。进一步的验证和分析表明,GRB10的PH域能够结合到PP2Ac催化亚单位。从机制上看,GRB10敲除后可增加PP2Ac蛋白的稳定性,进而降低AR S81的磷酸化并降低AR活性。
最后,研究人员指出,他们的研究结果表明GRB10和AR信号传导之间存在相互反馈,表明了GRB10在PCa进展中的重要性。
原始出处:
Jun Hao,Xinpei Ci,Yong Wang et al. GRB10 sustains AR activity by interacting with PP2A in prostate cancer cells. Int J Cancer. Oct 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#癌细胞#
32
#互作#
26
#前列腺癌细胞#
29
学习了
71
前列腺癌相关研究,学习了,谢谢梅斯
39