BMJ子刊:跨11年超45万人的前瞻性研究揭示健康成年人随机血糖与全因死亡率之间的关系
2021-11-06 MedSci原创 MedSci原创
RPG水平与CVD、CKD、慢性肝病、癌症和全因死亡率之间存在正对数线性关系,这种关系贯穿整个血糖检测范围,并在随访期间排除糖尿病患者后持续存在。
糖尿病是一系列血管性和非血管性疾病(包括缺血性心脏病(IHD)、中风、慢性肾脏病(CKD)和传染病)重要死亡风险因素。虽然已经有充分的证据表明,血糖水平低于糖尿病诊断阈值时,心血管疾病(CVD)的死亡风险较低,但与其他特定死亡原因的关系远未明确。
近几十年来,中国尿病和糖尿病前期的患病率显著迅速上升,突出了血糖作为危险因素的重要性。此外,中国许多主要慢性病的负担与西方人群有很大不同(例如,中风、慢性肝病和某些癌症造成的死亡率较高,而IHD死亡率相对较低)。因此,对中国血糖与病因特异性死亡率相关性的研究有望为这些相关性提供有价值的新证据,为疾病预测和预防工作提供信息。
本研究调查了中国无糖尿病成年人长期常规随机血糖(RPG)水平与死因特异性死亡风险之间的关系。2004-2008年,嘉道理生物库在中国10个地区招募了512891名30-79岁的成年人(59%为女性)。在基线调查和随后的随机幸存者调查中,参与者被采访和测量收集,包括现场RPG测试。死因是通过与当地死亡登记机构的联系确定的。
结果显示,在平均11年的随访中,452993名之前没有诊断出糖尿病或其他慢性病的参与者中有37214人死亡。RPG与全因、心血管疾病(CVD)(n=14209)和慢性肾病(CKD)(n=432)死亡率之间存在正的对数线性关系。在RPG<11.1 mmol/L时,每增加1.0 mmol/L常规RPG,全因校正HRs分别为1.14、1.16和1.44。正常RPG与慢性肝病和癌症死亡率呈正相关,但在基线RPG 11.1 mmol/L时风险相对较低。在排除随访期间发生糖尿病的参与者后,这些相关性持续存在。
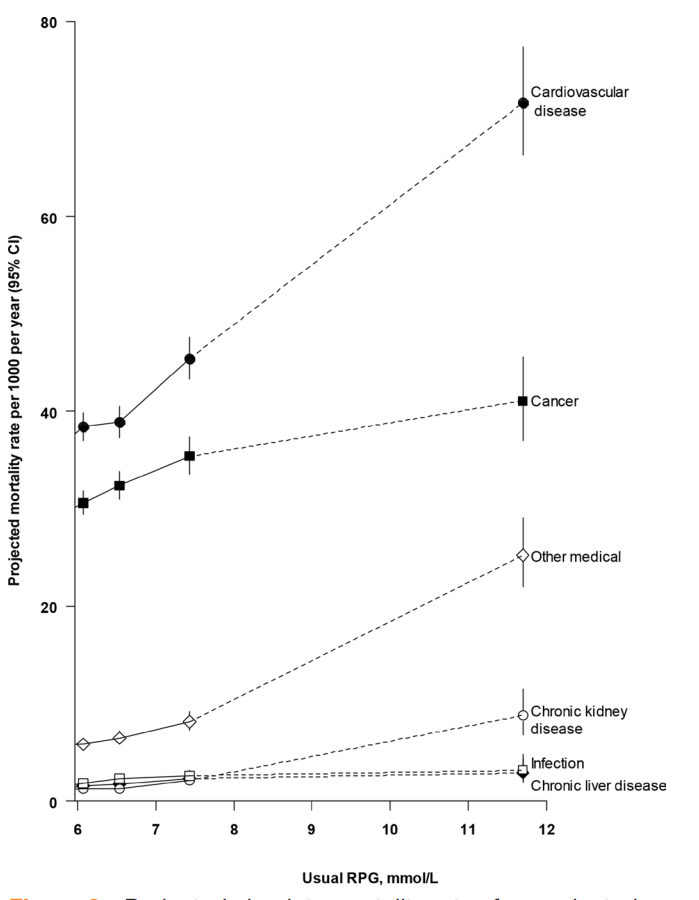
按通常随机血糖水平计算的选定主要疾病的预测绝对死亡率
总而言之,在无糖尿病的参与者中,RPG水平与CVD、CKD、慢性肝病、癌症和全因死亡率之间存在正对数线性关系,这种关系贯穿整个血糖检测范围,并在随访期间排除糖尿病患者后持续存在。这提供了潜在的病因学见解,并提示血糖可能为预测死亡风险提供有用的信息。其中许多关联的因果性质尚不清楚。然而,如果确定了,尽管RPG与死亡风险的关联相对较弱,但人群血糖水平的降低可以显著降低死亡率,特别是心血管疾病和癌症导致的死亡率。
参考文献:, et al. Random plasma glucose levels and cause-specific mortality among Chinese adults without known diabetes: an 11-year prospective study of 450,000 people
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMJ#
33
#前瞻性#
36
#前瞻性研究#
37
#全因死亡率#
45
赞
49