eLife:颠覆旧识!痴呆蛋白“变坏”比我们猜测的要“早”
2018-07-15 悠然 生物探索
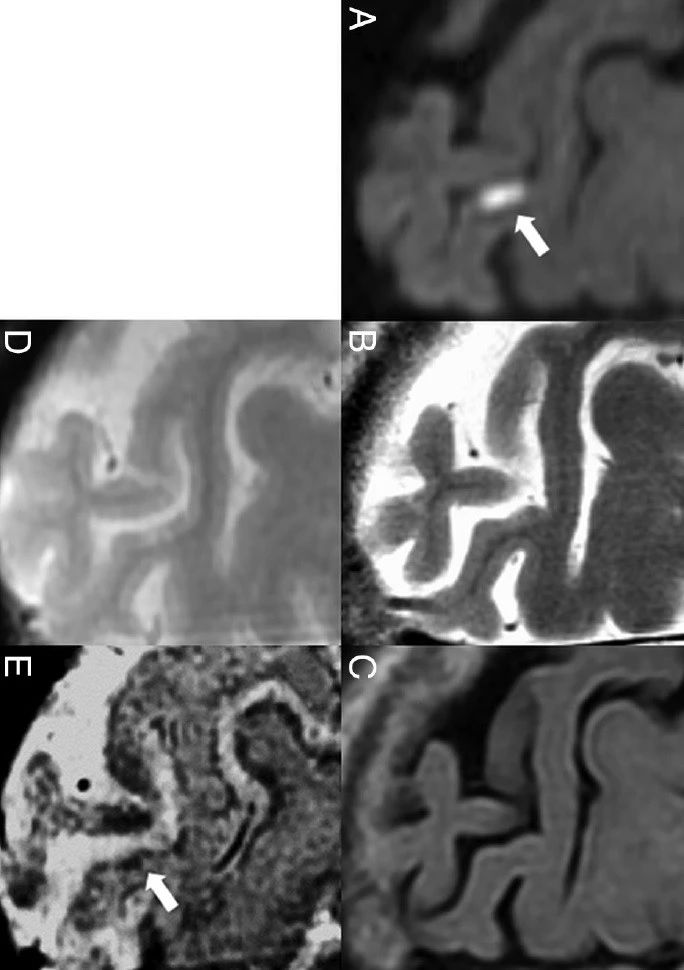
7月10日,《eLife》期刊以“Inert and seed-competent tau monomers suggest structural origins of aggregation”为题发表了这一项突破性成果。来自于德克萨斯大学西南医学中心的O'Donnell大脑研究所的科学家们解析了Tau蛋白在形成更大聚合体之前的“变形记”。这一发现为AD提供了一种新的策略——在Tau蛋白变坏之前将

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Life#
34
#eLife#
34
学习了.谢谢分享
57
学习了
52
阅
47
老年人痴呆何药可用??
33
学习了.长知识
44
学习了谢谢
54