Gastroenterology :鱼类脂肪酸或可降低肝癌风险
2012-05-24 爱唯医学网 爱唯医学网
近日,6月刊的《胃肠病学》(Gastroenterology )发表的一项以人口为基础的日本成人研究显示,食用富含n-3多不饱和脂肪酸(n-3 PUFA)的鱼类以及二十碳五烯酸(EPA)、二十二碳五烯酸(DPA)和二十二碳六烯酸(DHA)等n-3 PUFA与肝细胞癌(HCC)发生风险呈剂量依赖性负相关。 长期以来,食用n-3 PUFA被认为可降低多种癌症的发生风险,但对肝癌预防作用的专门研究报道

近日,6月刊的《胃肠病学》(Gastroenterology )发表的一项以人口为基础的日本成人研究显示,食用富含n-3多不饱和脂肪酸(n-3 PUFA)的鱼类以及二十碳五烯酸(EPA)、二十二碳五烯酸(DPA)和二十二碳六烯酸(DHA)等n-3 PUFA与肝细胞癌(HCC)发生风险呈剂量依赖性负相关。
长期以来,食用n-3 PUFA被认为可降低多种癌症的发生风险,但对肝癌预防作用的专门研究报道甚少。最近美国一项前瞻性研究表明,食用包括鱼类等“白肉”与肝癌呈负相关,但其他研究未发现上述相关性。为此,日本国家癌症中心的Norie Sawada博士及其同事利用上世纪90年代日本卫生部门开展的一项大规模队列研究数据,对90,296例成年人(基线年龄40~69岁)饮食数据进行详细分析,平均随访11年。
受试者完成一份有关上一年138种日常食物摄入的问卷调查,摄入量以标准份量或单位计算。其中19种食物涉及鱼类和贝类,包括咸鱼、干鱼、金枪鱼、鲑鱼或鳟鱼罐头、鲣鱼、金枪鱼、鳕鱼、海鲤鱼、鲭鱼、沙丁鱼、秋刀鱼、鱼子、鳗鱼、鱿鱼、章鱼、虾、蛤、螃蟹、田螺、以及各种鱼酱。研究者根据问卷计算每日鱼类消费量以及n-3 PUFA总摄入量和4种脂肪酸的具体摄入量,并分别计算鲑鱼、鳟鱼、海鲤鱼、鲭鱼、沙丁鱼、秋刀鱼和鳗鱼等富含n-3 PUFA鱼类的摄入量。在常规体检时采集血样,筛查丙型肝炎抗体和乙型肝炎表面抗原,以确定受试者是否携带丙型或乙型肝炎病毒。随访期间共计398例发生HCC。
结果显示,鱼类总摄入量与HCC风险呈弱负相关,最高vs.最低五分位数多变量危险比(HR)为0.64[95%置信区间(CI)为0.4~1.02,P=0.07]。若仅限于富含n-3 PUFA鱼类的摄入,则上述相关性达到统计学显著水平,HR为0.64(95% CI,0.42~0 .96;P=0.04)。HCC风险与EPA、DPA和DHA摄入量呈显著剂量依赖性负相关。校正年龄、性别、吸烟状况和体重指数后,上述相关性仍然存在,并且饮酒者和咖啡饮用者等亚组间也具有上述相关性。乙肝或丙肝阳性患者亚组食用富含n-3 PUFA鱼类与HCC风险也呈高度负相关。
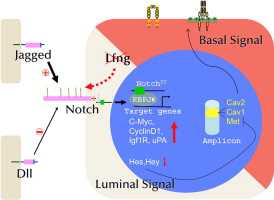
研究者指出,PUFA对肝癌保护作用的机理尚不清楚。鉴于HCC是一种与炎症有关的癌症,肝炎病毒或酒精等毒性化合物暴露可引起慢性炎症,推测PUFA的肝癌保护作用或许与其抗炎作用有关。
该研究的局限性表现为应估算鱼类和各种脂肪酸的摄入量,而不是直接测定其含量。此外,饮食数据仅来自于受试者一个时间点的自我报告。
该研究由日本国家癌症中心研究与开发基金会和厚生省资助。作者报告无相关利益冲突。(生物谷Bioon.com)

doi:10.1053/j.gastro.2012.02.018
PMC:
PMID:
Consumption of n-3 Fatty Acids and Fish Reduces Risk of Hepatocellular Carcinoma
Norie Sawada, Manami Inoue, Motoki Iwasaki, Shizuka Sasazuki, Taichi Shimazu, Taiki Yamaji, Ribeka Takachi, Yasuhito Tanaka, Masashi Mizokami, Shoichiro Tsugane
Background & Aims
Fish is a rich source of n-3 polyunsaturated fatty acids (PUFAs), such as eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). Although consumption of fish and n-3 PUFA has been reported to protect against the development of some types of cancer, little is known about its association with hepatocellular carcinoma (HCC).
Methods
We investigated the association between fish and n-3 PUFA consumption and HCC incidence (n = 398) in a population-based prospective cohort study of 90,296 Japanese subjects (aged, 45–74 y). Hazard ratios and 95% confidence intervals (CIs) for the highest vs the lowest quintile were estimated from multivariable adjusted Cox proportional hazards regression models. We also conducted subanalyses of subjects with known hepatitis B virus (HBV) or hepatitis C virus (HCV) status, and of subjects who were anti-HCV and/or hepatitis B surface antigen positive. All tests of statistical significance were 2-sided.
Results
Among all subjects, consumption of n-3 PUFA-rich fish and individual n-3 PUFAs was associated inversely with HCC, in a dose-dependent manner. Hazard ratios for the highest vs lowest quintiles were 0.64 (95% CI, 0.42–0.96) for n-3 PUFA-rich fish, 0.56 (95% CI, 0.36–0.85) for EPA, 0.64 (95% CI, 0.41–0.98) for DPA, and 0.56 (95% CI, 0.35–0.87) for DHA. These inverse associations were similar irrespective of HCV or HBV status.
Conclusions
Consumption of n-3 PUFA-rich fish or n-3 PUFAs, particularly EPA, DPA, and DHA, appears to protect against the development of HCC, even among subjects with HBV and/or HCV infection.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#癌风险#
27
#AST#
35
#GAS#
46
#Gastroenterol#
29
#Gastroenterology#
34