双侧肾上腺腺瘤型原发性醛固酮增多症
2013-07-25 卫生部北京医院泌尿外科 张亚群 朱生才 刘明 王建业 中国医学论坛报
图 T2WI磁共振影像[ A(左):右侧肾上腺肿瘤 B(右):左侧肾上腺肿瘤 ] 病例摘要 患者,男性,64岁,高血压20余年,3个月前出现头晕、肢体无力、周期性麻痹,昼间尿量800 ml,夜间尿量1000 ml。 血压为200/110 mmHg,血钾为2.4 mmo


图 T2WI磁共振影像[ A(左):右侧肾上腺肿瘤 B(右):左侧肾上腺肿瘤 ]
病例摘要
患者,男性,64岁,高血压20余年,3个月前出现头晕、肢体无力、周期性麻痹,昼间尿量800 ml,夜间尿量1000 ml。
血压为200/110 mmHg,血钾为2.4 mmol/L,血肌酐为112 μmol/L(正常值<97 μmo/L,以下括号内皆为正常值)。
卧位时:肾素水平为0.12 ng/(ml·h)(0.05~0.79),血管紧张素为58.8 pg/ml(28.2~52.2),醛固酮为426.7 pg/ml(48.5~123.5);立位时:肾素水平为0.36 ng/(ml·h)(0.93~6.56),血管紧张素为49.6 pg/ml(55.3~115.3),醛固酮为405.7 pg/ml(63~239.6)。
CT检查示左侧肾上腺占位性病变,直径为2.5 cm,右侧肾上腺占位性病变,直径为1.5 cm。磁共振成像(MRI)示双侧肾上腺外侧肢类圆形结节影,右侧约1.5 cm
×1.2 cm大小,左侧约2.6 cm×2 cm,边界清(图)。
诊疗过程
诊断
原发性醛固酮增多症(以下简称原醛症),双侧肾上腺占位,腺瘤可能性大。
结合以上立、卧位肾素-血管紧张素-醛固酮系统(RAAS)和CT、MRI影像学检查结果,可明确为双侧肾上腺占位,但不能完全确定双侧是否皆有功能。目前,18-羟皮质酮检测尚不普及,但该患者立位醛固酮水平与卧位基本持平,并未明显增加,符合腺瘤型原醛症的诊断(详见讨论部分)。
术前准备
应用硝苯地平控释片(30 mg/d)+福辛普利(10 mg/d)+琥珀酸美托洛尔缓释片(50 mg/d)+安体舒通(120 mg/d)四联降压药,控制血压并提高血钾水平。术前未应用皮质激素。入院1周后,血压控制在160/100 mmHg左右,血钾水平在3.5 mmol/L以上。
手术情况
入院第8日,于全麻下行双侧肾上腺部分切除术,经腹腔入路。术中以超声刀切断肾上腺,双侧均保留1/3左右正常肾上腺组织,止血确切。其中,左侧肿瘤较大,紧邻中央静脉,夹闭中央静脉后切除肿瘤,保留肾上腺上极正常组织;右侧肿瘤位于上极,夹闭中央静脉后切除肿瘤。两侧术区分别留置腹腔引流管1枚。术中出血合计少于50 ml,无术中并发症。
术后情况
腹腔引流管分别于术后第1天和第3天拔除,住院13天。手术当天及第1天,血压为160/100 mmHg左右,未应用降压药。术后第2天开始口服降压药硝苯地平控释片(30 mg/d)
+琥珀酸美托洛尔缓释片(50 mg/d),血压控制在150/90 mmHg左右,术后第1天血钾为3.7 mmol/L,术后未应用皮质激素替代治疗,无皮质醇功能不足表现。
术后病理
双侧均为肾上腺腺瘤,大小分别为3 cm×2.5 cm×2 cm, 2 cm×1.5 cm×1 cm,符合原醛症诊断。
术后随访
术后2个月随访,降压药为硝苯地平控释片(30 mg/d)+琥珀酸美托洛尔缓释片(50 mg/d),血压控制在140/90 mmHg左右,血钾为4~4.2 mmol/L。头晕、乏力和周期性麻痹症状消失,未出现发热、腹泻和厌食等皮质功能低下的表现,血皮质醇水平、节律及血促肾上腺皮质激素(ACTH)正常。
讨论
诊断 原醛症是体内醛固酮分泌增加、引起肾素分泌被抑制的综合征。国内由瑞金医院于1957年首次报告。临床上表现为高血压和低血钾,且一般认为高血压症状出现明显早于低血钾,从出现高血压到诊断为该病平均需7年4个月,而从出现低血钾到诊断则只需3年半。
原醛症病因有:① 肾上腺腺瘤,又称腺瘤型原醛症;② 肾上腺皮质癌;③ 原发性肾上腺皮质增生;④ 特发性肾上腺皮质增生;⑤ 糖皮质激素可抑制性原醛症;⑥ 异位产生醛固酮的肿瘤。
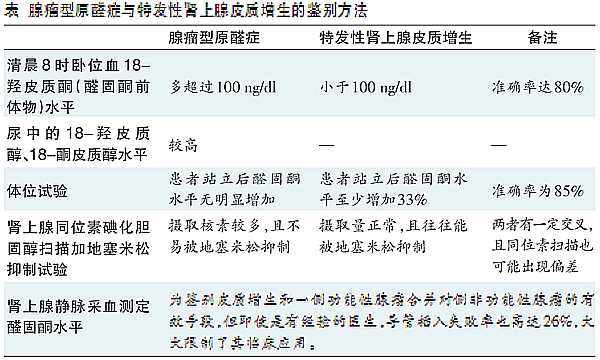
原醛症最常见病因是腺瘤型原醛症和特发性肾上腺皮质增生,两者合计占95%。在这两类病例中,病灶可位于单侧也可位于双侧,其中腺瘤型原醛症绝大多数都是单侧单发,双侧少见,有研究显示,腺瘤型原醛症双侧发病的比例不足2%。特发性肾上腺皮质增生也可双侧发生,且在影像学上与腺瘤区分有一定难度。腺瘤型原醛症主要以手术治疗为主,而特发性肾上腺皮质增生主要以药物治疗为主。因此,如何有效鉴别显得非常重要(表)。目前尚无准确性与特异性都令人满意的鉴别手段,甚至可能出现较大偏差,对于双侧肾上腺腺瘤的鉴别需进行多因素综合分析,有时甚至只能用术后病理结合临床表现及随访才能明确,期望在治疗前准确确定存在双侧肾上腺占位原醛症是很困难的,对双侧占位的功能性诊断也充满了不确定性。
治疗 尽管近来有以CT引导下射频治疗双侧肾上腺病变有效的报告,但多数学者仍认为腹腔镜下肾上腺切除术是治疗腺瘤型原醛症的金标准。
我们在手术前常规应用保钾型利尿剂联合其他降压药1~2周以控制血压,同时提高血钾水平达正常,结果显示,在手术过程中,患者血压波动很小,未出现心律失常情况,充分证明了控制血压、提高血钾是术前最重要的环节。
术中,双侧均采用夹闭中央静脉后切除腺瘤的方法。肾上腺血供丰富,有上、中、下三组动脉成梳齿状分支进入供血,保留的肾上腺组织不会因不规则切除而发生缺血坏死。肾上腺静脉血经中央静脉回流,但即使在阻断中央静脉后,也可经其他吻合支,甚至组织创面、接触组织的新生血管回流。
手术可采用双侧肾上腺全切后皮质醇替代治疗或保留肾上腺的肿瘤切除术。鉴于在双侧肾上腺全切后,皮质醇替代治疗往往引起骨质疏松和女性雄激素水平降低并导致相应并发症,保留肾上腺的肿瘤切除术对于提高患者生活质量意义重大。波尔皮利亚(Porpiglia)报告,双侧均保留1/3体积肾上腺时,患者术后出现轻度皮质功能低下症状,但不需替代治疗。腹腔镜下判断肿瘤和正常肾上腺组织界限相对容易,术中应尽可能保留正常组织,同时应尽量保持术野清晰,减少出血,这样则可清晰地判断腺瘤边缘和毗邻,能更多保留正常组织和减少周围误损伤发生。超声刀可在切断肾上腺组织同时有效止血,可很好地避免术中、术后大出血。
双侧肾上腺部分切除术后要十分注意肾上腺危象的发生,其中主要以急性肾上腺功能不全多见。临床表现发生率按从高到低排序为:临床情况的严重恶化、发热、腹痛或腰痛、低钠血症、低血压、腹胀、嗜睡和迟钝、高钾血症。
相对于我们认为最易发生的低血压(36%),发热发生率为70%,这尤应引起重视。因此,若发生相关症状,可应用小剂量ACTH试验明确是否有肾上腺危象发生,一旦证实,早期足量应用皮质激素替代治疗既有助于患者围手术期的恢复,也减少了长期副作用的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
21
#肾上腺#
31
#醛固酮增多症#
20
#醛固酮#
30
#双侧#
21