ISRD & ATS 2016:洪群英教授谈荧光支气管镜在肺癌早期诊断中的应用
2016-10-21 MedSci MedSci原创
14日下午,复旦大学附属中山医院呼吸科洪群英教授作了题为“荧光支气管镜在肺癌早期诊断中的应用”的精彩演讲。梅斯小编对洪群英教授的精彩报告进行整理,与大家分享。
2016年10月14日~16日,由中国健康促进基金会、上海市呼吸病研究所、国际呼吸学会等主办,美国胸科协会(ATS)和复旦大学呼吸病研究所等协办,上海梅斯医学承办的“第十二届上海国际呼吸学会暨ATS联合论坛”(ISRD & ATS 2016)在上海展览中心隆重举行。
14日下午,复旦大学附属中山医院呼吸科洪群英教授作了题为“荧光支气管镜在肺癌早期诊断中的应用”的精彩演讲。梅斯小编对洪群英教授的精彩报告进行整理,与大家分享。

复旦大学附属中山医院呼吸科洪群英教授
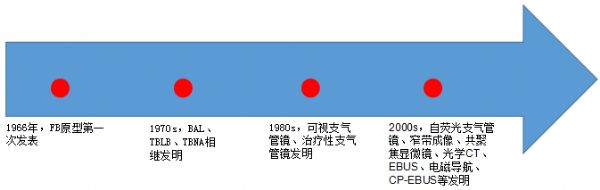
洪群英教授首先介绍了支气管镜的发展史,如下图:
然后,洪群英教授从以下七个方面讲述了荧光支气管镜。
一、荧光支气管镜的构造和功能:
自然界内有一些物质存在荧光现象,即在某特定波长光线的照射下,可以辐射出波长比原照射光线长的光,辐射出的波长较长的光线就是荧光。可用于观察气管、支气管黏膜荧光现象的支气管镜,就是荧光支气管镜。
二、荧光支气管镜的研制历史:
二、荧光支气管镜的研制历史:
1900年Wood发现在100瓦水银灯下组织可发生自身荧光;
1933年Sutro观察到水银灯照射下乳腺癌发生粉红色荧光、正常乳腺发生绿色荧光;
1989年加拿大哥伦比亚郡肿瘤研究所与Xillix公司研制出光诱导荧光支气管镜(LIFE)。1997年上市并不断改进研制了荧光支气管镜。
三、荧光支气管镜的结构:
荧光支气管镜一般都包含白光部分和荧光部分,使用时可以交替观察气道黏膜在白光下的表现和荧光影像。白光部分的结构和工作原理与普通支气管镜相同,荧光部分的结构根据采用的不同技术可以分为两大类:激光成像荧光支气管镜(Laser imaging fluorescence endoscopy, LIFE)和药物荧光/自荧光支气管镜(Drug induced fluorescence and autofluorescence D-Light/AF)。激光成像荧光支气管镜(LIFE)由激光发生装置、CCD摄像头、图像处理系统、监视器等组成。药物荧光/自荧光(D-Light/AF)支气管镜由照射光源、摄像系统、监视器和分光分析系统组成。
洪群英教授介绍说,目前临床应用的AFB主要有四家:
加拿大Lam等设计的LIFE系统,利用氦-镉激光装置产生蓝色激光,照射支气管产生红色和绿色荧光。
D-Light系统,有德国慕尼黑激光研究院设计,光源可产生普通光和两束蓝光,光强度显著高于LIFE系统,并增设一个外源性荧光观测系统。
日本PENTAX公司的SAFE系列,光源为氙光灯。
日本Olympus公司的AFI系列,光源为氙光灯。
四、自荧光支气管镜系统(lung imaging fluorescence endoscopy, LIFE)的工作原理:
不需要外源性光敏物质,波长405nm紫光或442nm蓝光照射支气管黏膜,将观察到的细胞自发荧光图像通过支气管镜连接到高分辨照相机,再转换成数据输入计算机。肿瘤与正常组织产生荧光强度有显著不同。自发性荧光支气管镜检查是利用细胞自发性荧光和电脑图像分析技术所开发的一种新型支气管镜:经光增强摄像机处理后,在荧光下,正常组织奖表现为绿色,而不典型增生、原位癌及浸润癌则表现为棕色或红褐色,可更准确地判断肿瘤的侵犯范围,可使支气管镜对肺癌及其癌前病变早期诊断的敏感性显著提高。
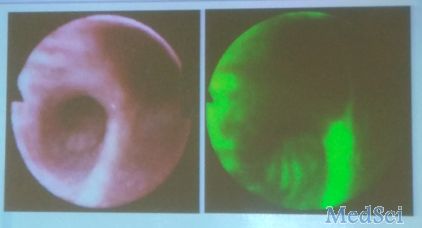
White-light bronchoscopy image LIFE bronchoscopy image
WLB与AFB区别:
原位癌和早期浸润癌病灶很小,表面直径只有几毫米,且在白光支气管镜下(WLB)缺乏特征性表现,因此,在WLB下常常难以发现(<5mm),白光支气管镜只能发现29%的原位癌。而荧光支气管镜可以发行WLB难以发现的病灶,尤其是癌前病变和原位癌,并对可疑部位进行定位活检和局部处理,从而可以提高肺癌早期诊断的阳性率和治愈率。
WBL分级:
Ⅰ级:先天解剖异常、外压性病变、单纯支气管间嵴增宽、黏膜色泽正常、不伴有充血水肿;
Ⅱ级:黏膜充血、水肿、增厚、色泽改变、血管聚集或扭曲;
Ⅲ级:黏膜颗粒样或明显新生物
AFB标准:
亮绿色:正常荧光
淡棕色(边界不清):荧光减弱-炎症,化生
棕红色(边界清楚):荧光缺失-异常增生,CIS
五、自荧光支气管镜操作方法(OLYMPUS BF TYPE F260)
原位癌和早期浸润癌病灶很小,表面直径只有几毫米,且在白光支气管镜下(WLB)缺乏特征性表现,因此,在WLB下常常难以发现(<5mm),白光支气管镜只能发现29%的原位癌。而荧光支气管镜可以发行WLB难以发现的病灶,尤其是癌前病变和原位癌,并对可疑部位进行定位活检和局部处理,从而可以提高肺癌早期诊断的阳性率和治愈率。
WBL分级:
Ⅰ级:先天解剖异常、外压性病变、单纯支气管间嵴增宽、黏膜色泽正常、不伴有充血水肿;
Ⅱ级:黏膜充血、水肿、增厚、色泽改变、血管聚集或扭曲;
Ⅲ级:黏膜颗粒样或明显新生物
AFB标准:
亮绿色:正常荧光
淡棕色(边界不清):荧光减弱-炎症,化生
棕红色(边界清楚):荧光缺失-异常增生,CIS
五、自荧光支气管镜操作方法(OLYMPUS BF TYPE F260)
(1)麻醉:局部麻醉,与常规支气管镜检查类似,因时间稍长,适当增加利多卡因剂量
(2)使用白光进行常规支气管镜检查,发现可疑部位,照相记录
(3)使用支气管镜控制部或者面板上的按钮进行荧光切换,不需中断操作,可立即获得荧光图像,对可疑部位进行活检。
(4)如常规支气管镜未发现病灶,则使用AFB再观察一遍。
六、自荧光支气管镜适应症:
利用正常组织、癌前病变、肿瘤三者自身荧光的差异,早期发现肿瘤,因此荧光支气管镜可用于:
(1)痰检筛查阳性的患者(绝对指征)
(2)影像学检查有肺癌可能者
(3)疑有原位癌可能者
(4)肺癌术后随访
(5)高危人群的普查(年龄>40岁,吸烟指数>600年支)
七、自荧光支气管镜评价:
(1)优势:提高肺脏的癌前病变及原位癌的早期诊断。Loewen等对169例患者联合荧光支气管镜和螺旋CT作为高危患者的肺癌筛查工具,66%的患者具有麟状上皮化生或者更严重的病变。在诊断第二位原发肿瘤、肺癌切除后边缘肿瘤残余、肺癌术后复发上也有优势。
(2)局限性:
- 只能检查较大的支气管,对中央型肺癌较为合适,而不适用于周围型肺癌。
- 灵敏度比普通支气管镜高,但有一定假阳性,特异性为30~60%。在285分取自异常光线发射区域的活检标本中只有95分包含异常的组织,即假阳性率可以高达66%。这种方法发现可疑病灶的现实意义还不清楚。
- 只能诊断中、重度不典型增生和癌变,而对增生和化生五特异性处理。
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ISRD#
45
#荧光#
47
#ATS#
0
#支气管#
50
很好,不错,以后会多学习
47
很好,不错,以后会多学习
58
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
45
谢谢分享一
55
#支气管镜#
47
#早期诊断#
26