原创Liwen RF(TM)射频消融及心肌活检系统带来肥心病诊治创新策略
2019-10-17 不详 美通社
空军军医大学西京医院肥厚型心肌病诊治中心刘丽文主任团队,联合诺诚医疗共同研发的Liwen RF™射频消融系统(以下简称Liwen RF™系统),在西京医院相继完成15台临床应用,手术过程顺利,患者恢复良好,这是“Liwen术式”在治疗肥厚型心肌病领域,首次融入2项全球首创的新技术 -- 可调射频消融针和心肌活检。“Liwen术式”+可调射频消融针 空军军医大学西京医院肥厚型心肌病诊治中心刘丽文主任
空军军医大学西京医院肥厚型心肌病诊治中心刘丽文主任团队,联合诺诚医疗共同研发的Liwen RF™射频消融系统(以下简称Liwen RF™系统),在西京医院相继完成15台临床应用,手术过程顺利,患者恢复良好,这是“Liwen术式”在治疗肥厚型心肌病领域,首次融入2项全球首创的新技术 -- 可调射频消融针和心肌活检。
“Liwen术式”+可调射频消融针
空军军医大学西京医院肥厚型心肌病诊治中心刘丽文主任团队,联合诺诚医疗研发的Liwen RF™射频消融系统,在西京医院相继完成15台临床应用,这是“Liwen术式”在治疗肥厚型心肌病领域,首次融入可调射频消融针和心肌活检这两项首创的新技术。
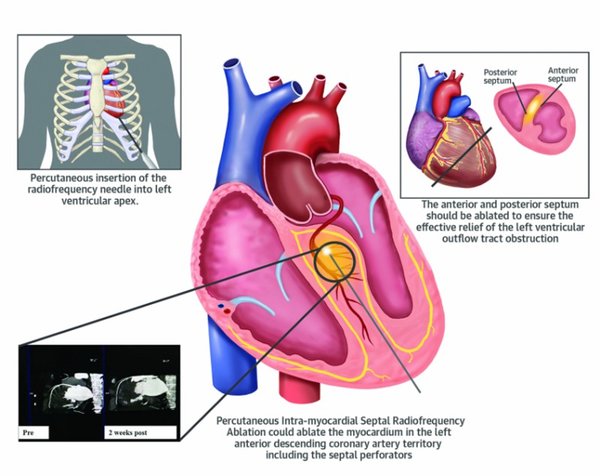
7月30日, 全球原创Liwen RF™系统手术成功实施,首例接受Liwen RF™系统治疗的患者术前为非对称性梗阻性肥厚型心肌病,整个手术完全在超声引导下完成,通过经胸经心肌微创介入方式进行,精准穿刺至室间隔肥厚部位,通过消融针的调节作用产生不同的消融范围,以达到精准消融,扩大左室流出道,缓解梗阻的效果。术中患者各项生命体征指标平稳, 术后症状明显改善。可调消融针能够根据病灶厚度实时调节消融范围大小,使得“Liwen术式”更加灵活、机动、安全,能够最大程度实现适形消融。
“Liwen术式”+心肌活检
8月6日,全球首例Liwen RF™射频消融同步心肌活检手术成功实施。手术过程中首次实施心肌活检,成功取得心肌标本,术中操作便捷,过程平稳顺利,患者术后恢复良好。
Liwen RF心肌活检是Liwen术式的最新临床应用,为心肌活检提供了一种新的路径。传统的心内膜活检操作复杂,且可能造成心内膜和传导束的损伤,而经心尖经心肌内的创新活检模式更为有效和安全,为疾病的临床指导与医学研究提供了宝贵的标本。
肥厚心肌知多少
肥厚型心肌病(hypertrophic cardiomyopathy, HCM)是最常见的遗传性心脏病,是以心肌肥厚、心室腔变小、心室血液充盈受阻和舒张期顺应性降低为基本特征的心肌病。肥厚型心肌病可起病于任何年龄,是青年人心源性猝死的首位病因和心力衰竭的主要原因之一。目前,肥厚梗阻型心肌病(HOCM)的治疗手段主要包括药物治疗、酒精室间隔消融及外科手术。西京医院刘丽文主任团队是目前国内专注于肥厚型心肌病诊疗的创新型医疗团队,超声引导下经皮心肌内室间隔射频消融术(Liwen术式)的成功开发和Liwen RF™系统技术的研发无疑为广大肥心患者带来了新的曙光。
Liwen RF™系统采用独创的手术路径,将装置在超声引导下经心尖经室间隔心肌内进行微创的诊断与治疗手段。Liwen RF™系统的治疗原理在于通过高频电波导致肥厚的心肌组织细胞内的离子产生热效应,进而导致肥厚的心肌细胞脱水坏死,同时Liwen RF™系统还可达到阻断肥厚心肌组织血液供应的效果。
与传统射频针对比,Liwen RF™系统的消融针的消融范围可根据室间隔的厚度自由调节,精准匹配预消融范围,微创,温和,适形消融,并且产品配置了活检针,能够经心尖经室间隔心肌行安全的心肌活检。并且独特的外针管设计,能够实现一次穿刺,多次消融、活检的操作。让手术更加简便、安全。
Liwen术式,是集创新性和有效性于一体的术式,一种安全、有效、微创心肌活检及治疗肥厚型心肌病的新策略。截止9月底,已经有141名肥厚型心肌病患者接受了“Liwen术式”的治疗,其中最近的15例是“Liwen RF™系统”率先用于临床诊断与治疗,效果良好。刘丽文主任团队在治疗肥厚型心肌病领域不断克服困难,突破瓶颈。医技合作,厚积薄发,碰撞新思维,发展新技术,Liwen术式“心”征程,肥心诊治迎曙光。
诺诚医疗是德诺医疗集团旗下新技术孵化公司,致力于为全球无法得到有效救治的肥心病患者提供安全有效的治疗方式。公司自主研发的Liwen RFTM系统,为肥厚型心肌病治疗提供了一种安全、有效、精确、微创的创新治疗策略。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#心肌活检#
27
#活检#
25
#射频消融#
41
#创新#
27
#消融#
31
#新策略#
32