癌症和慢性病治疗新策略
2015-07-10 孙学军 科学网
雷帕霉素属大环内酯类抗生素和免疫抑制剂,与FK506的结构相似,可阻断T淋巴细胞及其他细胞由G1期至S期的进程,从而发挥免疫抑制效应。起初雷帕霉素被研究作为低毒性的抗真菌药物,1977年发现雷帕霉素具有免疫抑制作用,1989年开始把雷帕霉素作为治疗器官移植的排斥反应的新药进行试用,目前III期临床试验正在进行之中。从临床应用来看,雷帕霉素有很好的抗排斥作用,且与环孢霉素A和FK506等免疫抑制剂有
雷帕霉素属大环内酯类抗生素和免疫抑制剂,与FK506的结构相似,可阻断T淋巴细胞及其他细胞由G1期至S期的进程,从而发挥免疫抑制效应。起初雷帕霉素被研究作为低毒性的抗真菌药物,1977年发现雷帕霉素具有免疫抑制作用,1989年开始把雷帕霉素作为治疗器官移植的排斥反应的新药进行试用,目前III期临床试验正在进行之中。从临床应用来看,雷帕霉素有很好的抗排斥作用,且与环孢霉素A和FK506等免疫抑制剂有良好的协同作用,是一种疗效好,低毒,无肾毒性的新型免疫抑制剂。

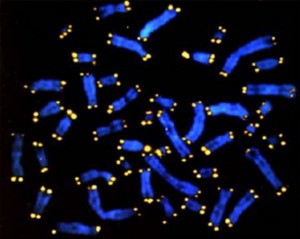
(1) Senescence signals activate IL-1α transcription; (2) IL-1α translation isMTOR-dependent and sensitive to rapamycin; (3) IL-1α atthe plasma membrane binds the IL1R; (4) IL1R occupancy activates IL1Rsignaling; (5) IL1R signaling releases IκB, allowing NF-κB translocation to thenucleus, where it activates the transcription of genes encoding SASP factors;(6) SASP factors are transcribed, translated and secreted.
科学家最近发现,间断使用雷帕霉素,可抑制癌症和慢性病的炎症反应。这种炎症被阻断后,需要一段时间才能重建。根据这一特点,采用间断给药方法,在实现抑制炎症的同时,减少雷帕霉素的用量,从而减少其副作用。该研究7月6日发表在Nature Cell Biology杂志上。
文章资深作者,Buck研究所的Judith Campisi教授说。“研究将为衰老性疾病和癌症治疗带来新思路,服药一段时间后可间隔几年后再服,不需要长期连续服药。”
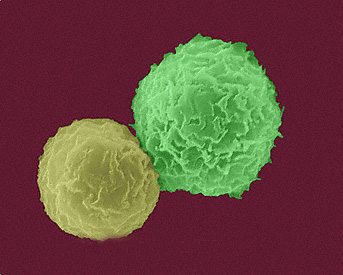
细胞和动物实验结果发现,雷帕霉素能抑制mTOR通路,减少衰老细胞分泌的炎症性细胞因子。

Rapamycin suppresses tumour cell growth.
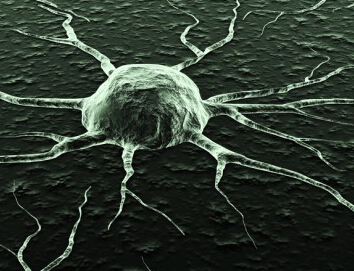
肿瘤化疗可损伤DNA,并导致肿瘤周围微环境内细胞发生衰老。Campisi说,虽然化疗能缩小瘤体,但也会导致肿瘤周围组织发炎。炎症信号也会促进癌细胞生长。雷帕霉素能阻止小鼠癌症复发。炎症驱动肿瘤生长可有效被雷帕霉素阻止,因此可以对这类患者开展临床研究。Fred Hutchinson 癌症研究中心Peter Nelson教授准备进行雷帕霉素与标准疗法联合治疗肿瘤的临床试验。试验希望针对性对特定类型的患者进行试验。
文章第一作者Remi-Martin Laberge博士说,雷帕霉素能阻断细胞产生白细胞介素质1α(IL-1),抑制IL-6基因表达,阻止该炎症因子合成。雷帕霉素能对炎症产生长期抑制,重启炎症回路需要很长时间。根据这一研究证据,这组科学家提出间断服药的颠覆性方式。
2014年完成的一项临床试验发现,雷帕霉素可增强老年人对流感疫苗的应答。作为免疫抑制剂,雷帕霉素也有易感染、高血糖和高血脂等副作用,长期用药更容易产生。
雷帕霉素也是一种公认的抗衰老药物,一般认为是通过抑制mTOR通路实现,但具体机制并不十分清楚。本研究结果发现,雷帕霉素间断给药能长期抑制炎症反应,这可能是该药物延长寿命的重要基础。因为炎症是许多衰老相关疾病如肥胖、动脉硬化、糖尿病、癌症等发生的共同基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗新策略#
30
看看
101
#慢性病#
40
#新策略#
30
看看
153