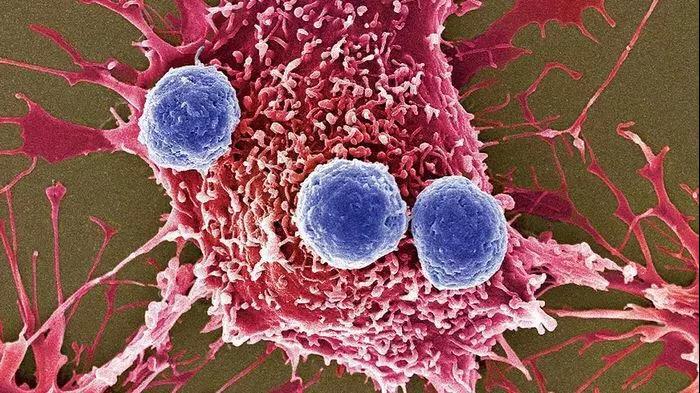
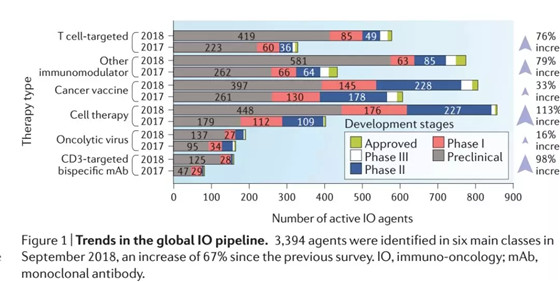
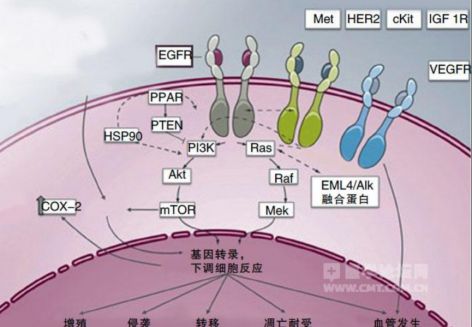
Nature Medicine:翻盘!多余脂肪悖论:肥胖虽然促发癌症,但却有助于癌症免疫疗法
2018-11-13 小通 生物通
“我们并没有推荐将肥胖作为改善癌症患者的预后。但肥胖诱导免疫抑制,促进肿瘤生成的作用机制,似乎真的可以通过检查点抑制剂免疫疗法逆转,翻盘。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CIN#
17
#Nat#
24
#DIC#
18
学习了谢谢
58
#Medicine#
24
#Med#
18
了解一下,谢谢分享!
44