Int J Hyper:加热化疗药物或可改善膀胱癌疗法
2016-05-18 生物谷 生物谷
日前,来自西班牙的研究人员发现,加热名为丝裂霉素C的化疗药物或可完全改变该药物的功效,此前丝裂霉素C用来治疗膀胱癌。

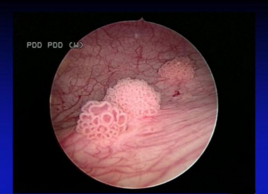
图片摘自:livescience.com
日前,来自西班牙的研究人员发现,加热名为丝裂霉素C的化疗药物或可完全改变该药物的功效,此前丝裂霉素C用来治疗膀胱癌,相关研究刊登于国际杂志the International Journal of Hyperthermia上。
这项研究发现是科学家们花费四年半时间的成果,他们设计的再循环高温膀胱内化学疗法(Recirculant hyperthermic IntraVEsical chemotherapy treatment,HIVEC)主要包括加热丝裂霉素C溶液,随后用水稀释直至温度达到43,载将药物溶液运输至膀胱中,在稳定压力下该药物每分钟可以循环200毫升,同时膀胱内的温度可以维持60分钟。40位膀胱癌患者参与到了这项研究计划中,他们被分为两组,其中一组在进行膀胱切除术前接受这种新型疗法(HIVEC),而另外一组在进行膀胱切除后接受该疗法。
其中97%的患者都可以完成整个HIVEC治疗过程,而且大部分的参与者对疗法反应良好,均表现出了较低的复发率,此外患者机体出现的副作用程度较低,而且对治疗计划的影响较小。大部分的膀胱癌患者都会通过内镜手术切除或肿瘤组织的切除来进行癌症治疗,然而有些患者则需要后期治疗,其中就包括膀胱周围的循环药物疗法,一旦疗法失败可选择的疗法就变得非常少了,除非移除膀胱。
常见的卡介苗疗法(Bacillus Calmette–Guérin,BCG)是一种非常有效的治疗非肌肉浸润性膀胱肿瘤的疗法,而丝裂霉素C效力并不如卡介苗,但研究者认为,对丝裂霉素C药物溶液进行加热可以部分增加药物的效力,而这或许归因于高温增加了药物的可溶性,同时部分也因为膀胱粘膜组织通透性的增加。
随后研究人员模拟了每位患者接受HIVEC疗法的成本节约情况,三年后患者大约可节约687欧元;更让研究者不可意思的是,当他们利用HIVEC疗法来治疗某些患者时,在大部分患者机体中肿瘤完全消失了,而且在接下来的几年里肿瘤并没有复发;这或许就表明,对于某些患者而言,HIVEC疗法或许是一种低侵入性的可替代疗法。
Alejandro Sousaa,et al.Recirculant hyperthermic IntraVEsical chemotherapy (HIVEC) in intermediate–high-risk non-muscle-invasive bladder cancer.the International Journal of Hyperthermia.doi:10.3109/02656736.2016.1142618
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
29
拜读,好文
63
#化疗药物#
25
#化疗药#
28
是这样的
79
值得收藏
106