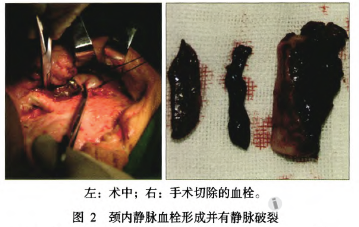
严重颈部坏死性筋膜炎并发颈内静脉血栓1例
2017-10-25 佚名 华西口腔医学杂志
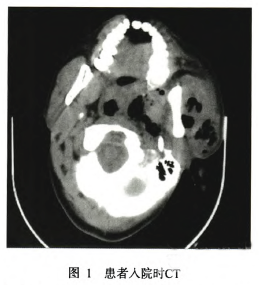
患者入院前10d出现左下后牙疼痛,未予治疗。6d出现左面部肿痛,体温升高,最高达38.5℃,于当地卫生所就诊,给予输液治疗4d(具体不详),肿痛进行性加重,出现寒战。1d前肿痛进一步向左面颈部弥漫,皮色发红,触痛明显,呼吸时稍费力,张口受限,吞咽困难,伴呛咳,来解放军第252医院就诊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#颈内静脉#
35
#并发#
30
#静脉血#
24
#静脉#
35
#坏死#
34
#坏死性筋膜炎#
32
#颈部#
26