华西医院完成西部地区首例Pentaray指导下高密度标测射频消融
2015-10-23 华西医院朱方 医学论坛网
10月21日,华西医院心脏内科成功完成西部地区首例Pentaray指导下高密度标测射频消融。 这位患有心房纤颤的老年患者,曾经接受过一次射频消融治疗。年龄大,心房里疤痕很多,现在又发生了房性心动过速,这类疤痕依赖性的房性心动过速,消融难度极大。常规的逐点消融费时费力,还要结合拖带等标测方法,成功率低。房颤消融术后房性心动过速,是困扰电生理学家的难题。解决这一难题的关键是建立高密度

10月21日,华西医院心脏内科成功完成西部地区首例Pentaray指导下高密度标测射频消融。
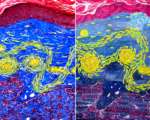
这位患有心房纤颤的老年患者,曾经接受过一次射频消融治疗。年龄大,心房里疤痕很多,现在又发生了房性心动过速,这类疤痕依赖性的房性心动过速,消融难度极大。常规的逐点消融费时费力,还要结合拖带等标测方法,成功率低。房颤消融术后房性心动过速,是困扰电生理学家的难题。解决这一难题的关键是建立高密度标测的方法,能在较短的时间内,在心腔内采集数百甚至上千点的数据信息,并采取特殊计算法则,精确显示局部病灶或者折返的关键峡部。但以往的线性或环状电极容易形成假腔,不能分辨近场及远场电位,有诸多缺陷。

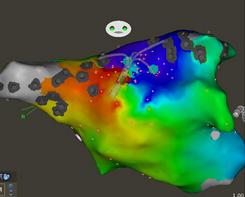
华西医院心内科电生理亚专业首次引进了美国强生公司的高密度标测设备——Pentaray,为复杂心律失常的治疗提供了崭新的解决方法。Pentaray是一种特殊的包含了五个分支的电极,每个分支包含了4个间距在2-6-2毫米的微小电极。每个分支的直径仅3F,可以轻松进入心腔内细小的皱褶。五个分支像章鱼的腕足一样伸开,十分柔软,可以紧密而又安全地贴靠到心内膜表面,记录到极为细微的电位,而这些电位可能在传统标测方法中会被认为是干扰而忽视。
心内科电生理亚专业付华教授和崔凯军教授为这位患者进行了左右心房的标测。每个心房的标测不超过两分钟,而且可以完全在不踩X线的情况下进行,大大保障了病人的安全。标测提示这是一例围绕左心房顶部进行折返的房速,付华教授仅用了1分钟即消融成功。
高密度标测设备为复杂心律失常,包括房颤、房速,尤其是器质性心脏病室性心动过速的消融提供了光明的前景。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#西医院#
27
#PE#
22
nice
107
nice
113
#射频消融#
29
#消融#
32
#华西#
25
也
120