Lancet:憋气并抬高双腿(改良Valsalva动作):能有效终止室上速!(附评论)
2015-11-04 徐媛&kelly MedSci原创
尽管标准Valsalva动作是室上速患者的一线急诊治疗方法,但其成功复律比例较低(5%~20%),本研究评估了改良的瓦尔萨尔瓦动作(Valsalva)治疗后恢复正常窦性心律的有效性。 研究人员在英格兰医院急诊科进行了一项随机对照、平行对照试验。研究人员按照1:1的比例将患者随机分配至标准Valsalva动作组和改良Valsalva动作组。研究人员纳入在2013年1月11号到2014年12月2

Valsalva动作,也称瓦氏试验,因其简单无创,是室上速患者的一线急诊治疗方法,但是由于做得不到位,成功率较低只有5%~20%。
而近期发表的REVERT研究改进了Valsalva动作:让患者在半卧位憋气之后立即平卧,并由他人抬高其双腿;而且证明这种改进很有成效。
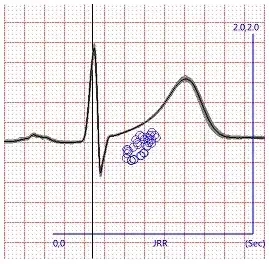
研究人员在英格兰医院急诊科进行了一项随机对照、平行对照试验。研究人员按照1:1的比例将患者随机分配至标准Valsalva动作组和改良Valsalva动作组。纳入在2013年1月11号到2014年12月29号期间的433名参与者,包括房颤和房扑患者。主要了解改变Valsalva动作的姿势是否可以改善治疗成功率,主要研究终点为干预后1分钟恢复窦性心律。在214名室上速急诊患者中,标准Valsalva仅使37(17%)例患者恢复正常窦律,而改良疗法使93(43%)例患者恢复正常窦律,达到显著差异校正比值比为3.7(95% CI 2·3-5·8; p<0·0001)。
研究表明,这一改进的Valsalva动作,较之传统半卧位可显著提高室上性心动过速的复律成功率。前者仅有17%成功恢复窦性心律,而改进动作后,治疗成功率达43.5%。
研究者对此很欣慰,因为通过简单调整姿势,就可使患者回心血量增加,从而增加Valsalva动作的成功治疗率,很有临床意义。从而也避免了一大部分患者不得已注射腺苷而产生的濒死感等不良反应。
然而这样一个简单的临床研究可以在Lancet上发表,不得不引起我们的深思。
研究的评论指出:每当提出一个新的可能的治疗标准时,都要评估它的风险和有效性。希波克拉底誓言的原则是永远不要给病人带来伤害,但这一原则日益受到现代医学和社会期望的挑战。尽管仍需要更多的观察,但Appelboam和他同事的研究表明了调整后的Valsalva试验将很快进入标准实践中。
Valsalva方法是众所周知的,但操作技术是多样的。通过实现使用一个标准的40mmHg的压力大小,其次是仰卧的定位和抬腿的高度,Appelboam和他的同事创造了微创的方法,极其简单的过程,却使得几乎50%的患者达到复律。
相比其他可选择的治疗室上性心动过速的方法,Valsalva试验的优点是无论在医院还在家中,都可以帮助识别积极治疗有效的人群。腺苷是经常使用的,但它非常昂贵,病人通常不愿意使用,大多数临床医生都希望可以尽量避免使用。其它的治疗,如钙通道阻滞剂、β受体阻滞剂、甚至电击,都有小的但很重要的发生不良事件的概率。改良的Valsalva试验易于操作、便宜、非侵入而且可以重复;因此,所有病人在进行侵入性治疗前尝试进行这样一个标准的治疗是合理的。
临床医生往往因为各种客观因素对论文写作带有恐惧心理,但其实首先要清楚知道SCI期刊中发表的文章种类多样,如:综述、纯理论性的结果、新的仪器与方法介绍、案例报道以及实验研究成果,当然也包括对现有技术的改良和革新等。
将临床工作中积累的经验和成果进行总结并转化为理论,指导更多的临床实践和规范化操作,是作为一个好医生义不容辞的责任,也是现代社会对“新好”医生的要求。
我们无法否认论文发表在学术界和推动科技发展的重要作用,发表出好的文章也是有经验和方法可寻的。期望各位可以在MedSci的平台得到启发,并将更多更新的临床结果展现给大家,欢迎各位同仁来MedSci临床学院授课,整合资源,共同改进国内的医疗质量和推动中国医疗的发展。
参考来源:
Appelboam,Reuben,Mann, et al, REVERT trial collaborators.Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised controlled trial.Lancet. 2015 Aug 24
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#憋气#
30
#Lancet#
25
#Valsalva#
36
#室上速#
33
Ok
101
今后可在临床工作中应用。
69
嗯,好好学习
153