Autophagy:肿瘤相关TGFB1的非常规分泌方式
2018-01-08 海北 MedSci原创
TGFB1(转化生长因子β1)是在发育,纤维化和癌症中发挥驱动作用的潜在细胞因子。它被合成为前结构域生长因子复合物,其需要连接到LTBP(潜伏的转化生长因子β结合蛋白),然后被有效地分泌到细胞外的空间中去。
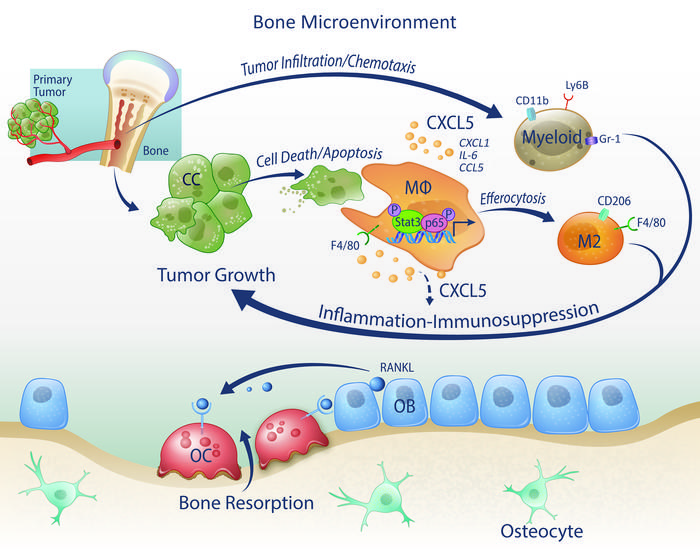
TGFB1(转化生长因子β1)是在发育,纤维化和癌症中发挥驱动作用的潜在细胞因子。它被合成为前结构域生长因子复合物,其需要连接到LTBP(潜伏的转化生长因子β结合蛋白),然后被有效地分泌到细胞外的空间中去。TGFB1被释放后,这种巨大的潜伏复合物能够被锚定到细胞外基质(ECM)网络,而后,成熟的生长因子需要被激活,以便结合其受体,并启动信号传导。
近日,来自德国科隆大学的研究人员发现了一种新的细胞内分泌途径。通过该途径,潜伏的TGFB1复合物到达质膜,并从成纤维细胞(组织修复过程,纤维化,和肿瘤基质的关键效应细胞)中被释放。其发现了一种潜伏状态的TGFB1是通过ILK(整合素连接的激酶)被成纤维细胞 - ECM通讯来调节的,ILK通过与ARHGAP26 / GRAF1相互作用来限制RHOA的活性。其他选定的细胞因子的分泌并不通过该形式。
潜伏的TGFB1与GORASP2 / GRASP55相互作用,并在由RAB8A依赖性途径分泌的MAP1LC3阳性自噬体中被检测到。有趣的是,如果人和小鼠成纤维细胞和巨噬细胞中缺乏自噬机制的关键成分,TGFB1的分泌被完全消除。
因此,研究人员的数据表明,TGFB1的非常规分泌模式增加了其生物利用度和活性在另一个水平的控制。
原始出处:
Julian Nüchel et al. TGFB1 is secreted through an unconventional pathway dependent on the autophagic machinery and cytoskeletal regulators. Autophagy, 2018. DOI: https://doi.org/10.1080/15548627.2017.1422850
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#分泌#
0
#TGFb#
52
#TGF#
36
肿瘤相关TGFB1的非常规分泌方式.
68
肿瘤相关的治疗.
85
非常好的文章.学习了
67
学习了.谢谢.
63
谢谢分享.学习了
67