Nat Chem Biol:一种抑制VCP酶的化合物或可用于癌症治疗
2013-08-19 佚名 bio360
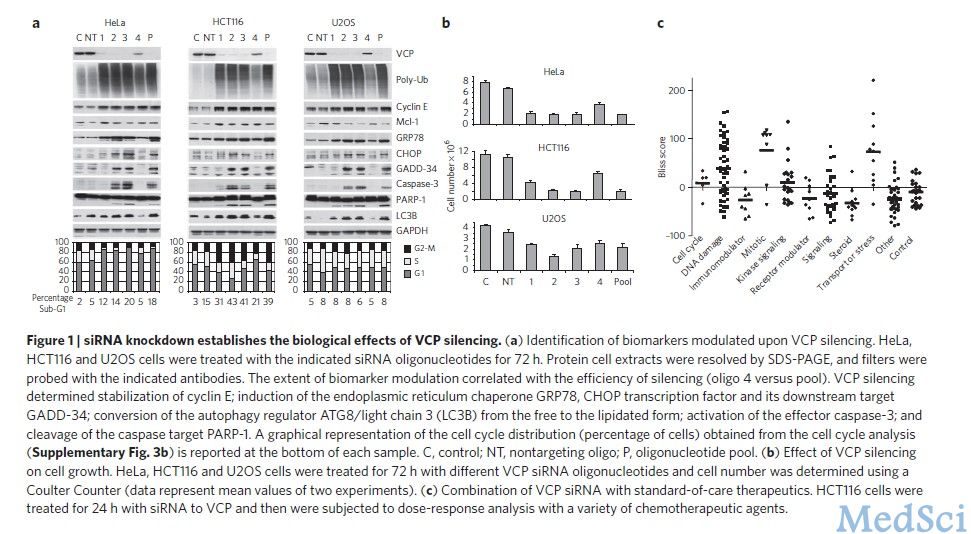
日前,意大利科学家发现,一种抑制VCP酶的化合物可为治疗癌症提供新工具。相关研究论文刊登在了《自然-化学生物学》(Nature Chemical Biology)杂志上。【原文下载】 VCP又名p97或Cdc48,是一种ATP酶(利用ATP裂解产生的能量完成其他反应的酶),在蛋白质的可控降解中起着重要作用。 科学家逐渐发现VCP也与癌症有一定联系:其功能对保持癌细胞健康是必需的。因而,

日前,意大利科学家发现,一种抑制VCP酶的化合物可为治疗癌症提供新工具。相关研究论文刊登在了《自然-化学生物学》(Nature Chemical Biology)杂志上。【原文下载】
VCP又名p97或Cdc48,是一种ATP酶(利用ATP裂解产生的能量完成其他反应的酶),在蛋白质的可控降解中起着重要作用。
科学家逐渐发现VCP也与癌症有一定联系:其功能对保持癌细胞健康是必需的。因而,抑制VCP功能可防止正常蛋白的降解并导致意外序列的产生,最终促使癌细胞死亡。
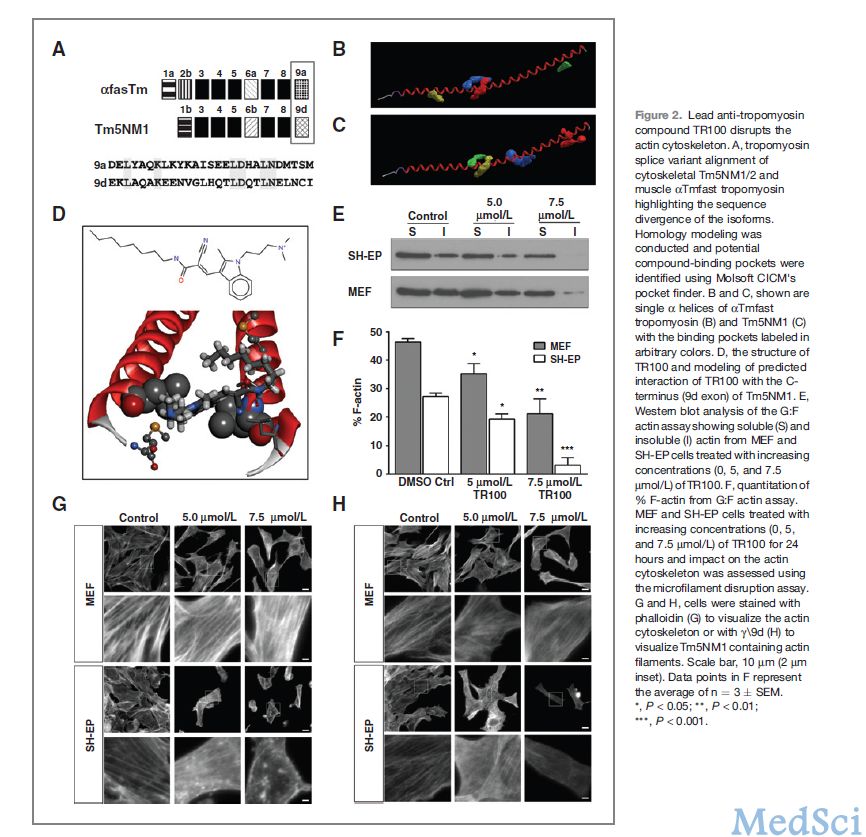
在这项研究中,研究人员发现一类合成化合物能通过三种不同的机制抑制 VCP。其中一组化合物跟ATP一样会与相同的位点结合,这组化合物与已知的 VCP抑制剂类似,但对VCP不具有选择性。
另外两组化合物则在新的方式下产生作用:一组会与ATP位点内的蛋白质形成共价键,而另一组则会与远离ATP位点的一个意外的变构位点相结合,可能是为了通过阻止催化所需的构型变化这种方式来关闭VCP的功能。
研究小组表示,这两组名为NMS-859和NMS-873的化合物可以导致癌细胞系中的细胞死亡。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Bio#
32
#癌症治疗#
26
#Biol#
23
#化合物#
23
#Nat#
30